In the evolving landscape of healthcare, ensuring seamless patient care across different settings is paramount. As healthcare systems embrace electronic health records and strive for improved patient outcomes, the concept of a Longitudinal Care Plan (LCP) has emerged as a potentially transformative solution. But what is a longitudinal care program, and why is it gaining traction in the medical field? This article delves into the essence of LCPs, exploring their potential to revolutionize patient care coordination and the current challenges hindering their widespread adoption.
Decoding Longitudinal Care Plans: A Comprehensive Overview
A Longitudinal Care Plan (LCP) is envisioned as a dynamic, patient-centric, and all-encompassing blueprint that documents a patient’s health journey over time. It’s more than just a static record; it’s a living document that evolves with the patient’s changing needs, goals, and preferences. Think of it as a roadmap guiding healthcare providers and patients alike towards optimal health and wellness across the continuum of care.
Key characteristics of an LCP include:
- Holistic Approach: An LCP considers the patient as a whole, encompassing not just their current illness but also preventive care, long-term goals, and overall well-being.
- Dynamic and Adaptable: Unlike traditional care plans that might be setting-specific, an LCP is designed to be continuously updated and adapted as the patient transitions between different healthcare settings like hospitals, skilled nursing facilities, and home healthcare.
- Patient-Centered: At its core, an LCP prioritizes the patient’s values, preferences, and goals. It’s built on bidirectional communication, ensuring the patient is an active participant in their care journey.
- Integrated and Accessible: Ideally, an LCP leverages electronic systems to consolidate information from various sources, creating a unified view accessible to all relevant providers and the patient themselves.
- Actionable Information: An effective LCP provides clear, actionable information that helps healthcare teams identify and achieve the individual’s health and wellness objectives.
Image alt text: Interdisciplinary healthcare team collaboratively reviewing a patient’s longitudinal care plan on a digital interface, emphasizing teamwork and coordinated care.
The Critical Need for Longitudinal Care Programs in Today’s Healthcare
The necessity for LCPs arises from significant gaps in communication and coordination that plague current healthcare systems, particularly during care transitions. These gaps pose serious threats to patient safety and the efficiency of care delivery.
Challenges Stemming from Lack of LCPs:
-
Fragmented Information: Without a central LCP, patient information becomes scattered across different systems and settings. This lack of information continuity can lead to:
- Incomplete or Ambiguous Data Transfer: Crucial details about a patient’s condition, medications, or care goals may be missing or unclear when they move between care settings.
- Care Delays and Errors: Providers in new settings may lack the necessary information to make timely and informed decisions, potentially causing delays in treatment or even medical errors.
- Increased Provider Stress: The burden of seeking clarification and piecing together fragmented patient information adds to provider workload and stress.
- Higher Rehospitalization Risks: Poor communication during transitions can lead to inadequate follow-up care and increased risk of patients being readmitted to hospitals.
-
Patient and Family Disengagement: Patients and their families often feel lost and uninformed during care transitions. Lack of involvement in care planning and insufficient information sharing can lead to:
- Anxiety and Confusion: Patients may be unsure about their treatment plans, medications, or follow-up appointments.
- Reduced Adherence: Without a clear understanding of their care plan, patients may struggle to adhere to recommendations, impacting their health outcomes.
- Unsafe Transitions: Jeffs et al.’s research highlights that lack of information and patient involvement are major threats to safe care transitions.
Longitudinal Care Plan vs. Plan of Care: Clarifying the Terminology
It’s important to distinguish between a Longitudinal Care Plan (LCP) and a “plan of care,” as these terms are sometimes used interchangeably, causing confusion. The Standards and Interoperability (S&I) Framework offers a helpful distinction:
- Longitudinal Care Plan (Care Plan): This is the overarching, long-term blueprint that encompasses all aspects of a patient’s care across all settings and involves all members of the care team, including the patient. It prioritizes concerns, goals, and interventions at a high level.
- Plan of Care (POC): This is more focused and discipline-specific. A patient may have multiple POCs, each tailored to a particular setting (e.g., acute care POC, home care POC) or discipline. These POCs should ideally be reconciled and integrated into the overarching LCP.
- Treatment Plan: Even more granular, a treatment plan focuses on a single health concern and is typically managed by one clinician (e.g., physical therapy treatment plan).
Think of it as a hierarchy: a single LCP can encompass multiple plans of care, which in turn may include various treatment plans. The LCP acts as the master document, ensuring all these different plans are coordinated and aligned with the patient’s overall health goals.
Image alt text: Table visually differentiating between Care Plan, Plan of Care (POC), Treatment Plan, and related definitions, emphasizing the hierarchical structure of longitudinal care planning.
The Agency for Healthcare Research and Quality (AHRQ) Care Coordination Framework and LCPs
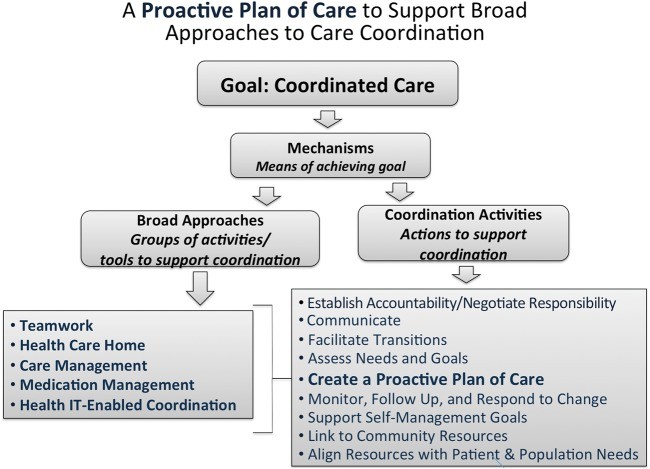
The Agency for Healthcare Research and Quality (AHRQ) Care Coordination Framework provides a valuable structure for understanding how LCPs fit into the broader context of care coordination. This framework emphasizes five “Broad Approaches” to achieve high-quality, patient-centered healthcare:
- Teamwork Focused on Coordination: LCPs necessitate a collaborative, interdisciplinary approach involving all care team members and the patient.
- Health Care Home (HCH): The LCP can serve as a central tool within the HCH model, ensuring coordinated and comprehensive primary care.
- Care Management: LCPs are essential for effective care management, supporting processes like case and disease management across settings.
- Medication Management: Medication reconciliation and management are crucial components of an LCP, ensuring medication safety during transitions.
- Health IT-Enabled Coordination: Technology plays a vital role in enabling LCPs, facilitating information sharing and communication across the care continuum.
The AHRQ framework highlights that creating a plan of care is just one of nine key activities supporting care coordination. However, for this plan to be truly effective, it needs to transcend individual settings and function as a longitudinal care program, connecting these “Broad Approaches” and facilitating seamless transitions.
Image alt text: Diagram of the AHRQ Care Coordination Framework, illustrating the five Broad Approaches and nine activities, emphasizing the role of longitudinal care plans in enabling coordinated care.
Current State and Challenges in LCP Implementation
Despite the recognized benefits, the widespread adoption of LCPs faces significant hurdles. Research indicates that LCPs are not yet a standard practice in many healthcare settings. A study involving professionals across various care settings revealed that:
- LCPs are Largely Absent: Participants reported that true LCPs, as envisioned, do not exist in their current systems.
- Fragmented Care Plans: While care plans of some form are present within individual settings, they are rarely shared or reconciled across different settings.
- Communication Gaps: Significant variation exists in the type and format of care plan information communicated during transitions.
- Outdated Technology: Even within integrated healthcare systems, communication often relies on outdated methods like paper and fax, hindering seamless electronic information exchange.
Barriers to Widespread LCP Adoption:
- Lack of Clarity and Standardization: Inconsistent definitions, nomenclature, and standards surrounding LCPs create confusion and hinder interoperability.
- Regulatory and Governance Issues: Lack of clear regulatory requirements, care plan governance, and defined ownership contribute to slow adoption.
- Workflow and Practice Challenges: Integrating LCPs into existing workflows and establishing patient-centered collaboration processes remain significant challenges.
- Technological Limitations: Limited interoperability between different health IT systems and lack of sophisticated tools to support LCP generation, sharing, and reconciliation are major obstacles.
- Minimal Meaningful Use Requirements: Current “Meaningful Use” incentives primarily focus on acute and outpatient settings, with minimal requirements for LCP components and limited incentives for adoption outside these settings.
Moving Forward: Transforming the Vision of LCPs into Reality
Realizing the full potential of Longitudinal Care Programs requires a concerted effort to overcome existing barriers and transform the LCP from an aspirational concept into a practical reality. Key strategies for the future include:
- Standardization and Interoperability: Developing and adopting standardized LCP definitions, data elements, and exchange formats is crucial for seamless information sharing across systems. The S&I Framework provides a valuable starting point.
- Technological Advancements: Investing in and implementing interoperable health IT systems with robust functionalities to support LCP creation, maintenance, and exchange is essential.
- Workflow Integration and Best Practices: Developing and disseminating best practices for integrating LCPs into clinical workflows, emphasizing patient-centered collaboration and care plan reconciliation, is vital.
- Policy and Incentives: Policy changes and incentive programs are needed to encourage LCP adoption across all healthcare settings, not just acute and ambulatory care. Future stages of “Meaningful Use” should incorporate more comprehensive LCP requirements.
- Patient Engagement: Actively engaging patients and families in the LCP development and update process, providing them with access to their LCPs, and utilizing patient portals and other technologies to facilitate communication are key.
- Rebranding and Marketing: “Rebranding” and effectively “marketing” LCPs with user-friendly tools and workflows can promote wider adoption by all care team members, including patients.
Conclusion: The Promise of Longitudinal Care Programs
What is a longitudinal care program? It’s more than just a care plan; it’s a paradigm shift in healthcare delivery. Longitudinal Care Programs represent a vital step towards achieving truly coordinated, patient-centered care. By breaking down information silos, fostering communication, and empowering patients, LCPs hold the promise of improving patient safety, enhancing care quality, and ultimately achieving better health outcomes. While significant challenges remain, the ongoing efforts to define, standardize, and implement LCPs offer a clear path towards a future where healthcare is more connected, efficient, and focused on the individual patient’s journey.
References
[1] Reference 1 from original article
[2] Reference 2 from original article
[3] Reference 3 from original article
[4] Reference 4 from original article
[5] Reference 5 from original article
[6] Reference 6 from original article
[7] Reference 7 from original article
[8] Reference 8 from original article
[9] Reference 9 from original article
[10] Reference 10 from original article
[11] Reference 11 from original article
[12] Reference 12 from original article
[13] Reference 13 from original article
[14] Reference 14 from original article
[15] Reference 15 from original article
[16] Reference 16 from original article
[17] Reference 17 from original article
[18] Reference 18 from original article
[19] Reference 19 from original article
[20] Reference 20 from original article
[21] Reference 21 from original article
[22] Reference 22 from original article
[23] Reference 23 from original article
[24] Reference 24 from original article
[25] Reference 25 from original article
[26] Reference 26 from original article
[27] Reference 27 from original article
[28] Reference 28 from original article
[29] Reference 29 from original article
[30] Reference 30 from original article
[31] Reference 31 from original article
[32] Reference 32 from original article
[33] Reference 33 from original article
[34] Reference 34 from original article
[34a]Reference 34a from original article
[35] Reference 35 from original article
[36] Reference 36 from original article
[37] Reference 37 from original article
[38] Reference 38 from original article
[39] Reference 39 from original article
[40] Reference 40 from original article
[41] Reference 41 from original article
[42] Reference 42 from original article
[43] Reference 43 from original article