Vision impairment disproportionately affects Indigenous populations in high-income countries, creating a significant health disparity. The question “Is The Aboriginal Eye Care Program Real?” underscores a critical need to understand the reality of eye care access for these communities. This article delves into the existing landscape of service delivery models aimed at bridging this gap, examining their effectiveness and highlighting areas for crucial improvement. Drawing upon a comprehensive review of published research, we shed light on the efforts underway and the path forward to ensure equitable eye health for Indigenous peoples.
Understanding the Landscape of Indigenous Eye Care Services
Indigenous populations globally face poorer health outcomes compared to their non-Indigenous counterparts, and eye health is no exception. Avoidable vision impairment, often stemming from conditions like cataract and refractive error, is more prevalent in Indigenous communities. This disparity is not inevitable; it’s largely driven by systemic barriers hindering access to timely and appropriate eye care services. To address this, various service delivery models have emerged, particularly in high-income nations committed to reducing health inequalities.
The real question isn’t whether “aboriginal eye care programs” exist, but rather, what is the scope, effectiveness, and cultural relevance of these programs? Our review of studies across Australia, the USA, Canada, New Zealand, Taiwan, and Greenland reveals a focused yet still limited body of work. Much of the research centers on Australia, with a significant emphasis on diabetic retinopathy screening. This focus, while important, doesn’t fully encompass the broader spectrum of eye health needs within Indigenous communities.
Key Areas of Focus in Existing Programs
The service delivery models identified can be broadly categorized, revealing common strategies and areas of concentration:
- Teleophthalmology: A prominent model, particularly for diabetic retinopathy screening. This approach utilizes technology to bridge geographical barriers, bringing specialist eye care closer to remote communities. Many programs integrate teleophthalmology into existing primary care settings, leveraging community health centers and Indigenous healthcare clinics. Mobile teleophthalmology units further extend reach, visiting communities directly.
- Integration into Primary Healthcare: Recognizing the importance of holistic care, several models focus on embedding eye care services within existing Indigenous primary healthcare systems. This integration can encompass various services, from optometry and refractive error correction to cataract surgery pathways and general eye health programs.
- Outreach Services: Bringing eye care professionals directly to communities through outreach initiatives is another vital strategy. Mobile eye clinics and visiting specialists overcome geographical barriers, delivering essential services in remote and underserved areas.
- Training Indigenous Health Workers: Empowering local communities is central to sustainable healthcare solutions. Training Indigenous health workers in primary eye care and specific skills like retinal imaging enhances service delivery and cultural appropriateness.
- Eye Health Promotion: Preventative care is paramount. Eye health promotion programs, often utilizing culturally tailored materials and methods, aim to raise awareness, improve knowledge, and encourage proactive eye care seeking behaviors within Indigenous communities.
- Trachoma Control: In specific regions, trachoma remains a concern. Dedicated programs employing the SAFE strategy (Surgery, Antibiotics, Facial cleanliness, Environmental improvement) target trachoma elimination through integrated interventions.
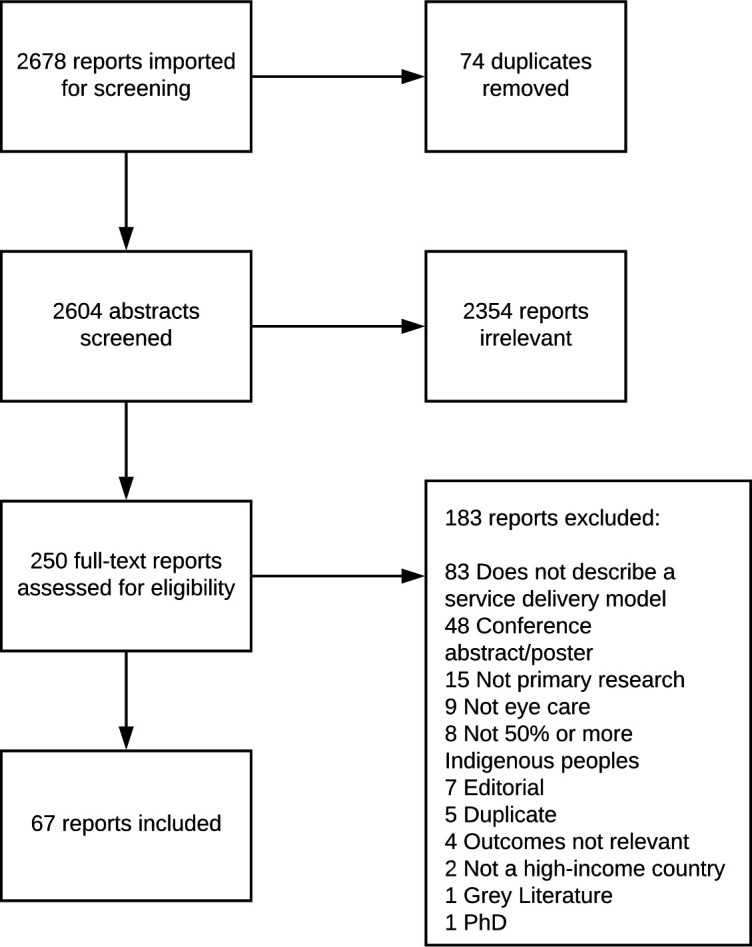
Image alt text: PRISMA flow diagram illustrating the study selection process for a review of Indigenous eye care service delivery models. The diagram visually outlines the number of abstracts screened, full-text articles assessed, and studies ultimately included in the analysis, providing transparency to the research methodology.
Are These Programs Effective? Measuring Impact and Outcomes
While the existence of Indigenous eye care programs is evident, assessing their effectiveness is crucial. Many studies report positive outcomes, often focusing on increased service utilization, such as higher screening rates and more spectacles dispensed. Teleophthalmology models, for instance, have demonstrated success in expanding diabetic retinopathy screening coverage in remote areas. Integration models have shown improvements in cataract surgery completion rates and overall eye care attendance.
However, a critical gap exists in rigorous, long-term evaluations. Few studies comprehensively assess the impact of these programs on the actual burden of vision impairment within Indigenous populations. Outcome measures often center on service outputs rather than the ultimate goal of improved eye health and reduced vision loss. Furthermore, the methodological approaches used to evaluate these interventions could be strengthened to provide more robust evidence of their effectiveness.
The Crucial Element: Cultural Sensitivity and Community Engagement
Beyond mere access, the cultural appropriateness and acceptability of eye care services are paramount for Indigenous communities. A significant finding is that while many programs aim to improve access, fewer explicitly address cultural sensitivity or actively engage Indigenous communities in service design and implementation.
Culturally sensitive approaches recognize and respect the unique values, beliefs, and practices of Indigenous peoples. Examples of culturally appropriate strategies include:
- Employing Indigenous health workers and eye health coordinators who understand the community and can build trust.
- Adapting service delivery models to incorporate cultural activities and rituals, creating a more welcoming and familiar environment.
- Developing health promotion materials that are linguistically and culturally relevant, using Indigenous languages and imagery.
- Establishing partnerships with Indigenous communities, leaders, and organizations to ensure services are community-driven and responsive to local needs.
Image alt text: Levesque’s framework of patient-centered healthcare access dimensions applied to Indigenous eye care models. The diagram maps various components of identified service delivery models onto the framework’s stages – Approachability, Acceptability, Availability, Affordability, and Appropriateness – illustrating how different programs address these key access dimensions for Indigenous populations.
Studies highlight that programs incorporating cultural sensitivity and community engagement demonstrate greater success in improving access and uptake. For instance, community-based teleophthalmology clinics with culturally relevant elements have shown higher attendance rates. When Indigenous communities are involved as stakeholders in program design, services are more likely to be effective and sustainable.
Bridging the Gaps and Moving Forward
The review underscores several key areas for future development and research to strengthen Indigenous eye care programs:
- Expand Geographical and Clinical Scope: Research and program development need to extend beyond Australia and diabetic retinopathy screening. Other high-income countries with Indigenous populations require attention, and service models should address the full spectrum of eye conditions prevalent in these communities, particularly cataract and refractive error, the leading causes of vision impairment.
- Prioritize Cultural Responsiveness and Engagement: Moving beyond simply providing services, programs must prioritize cultural safety and actively involve Indigenous communities in all stages, from design to implementation and evaluation. Frameworks for culturally responsive service delivery should be adopted and implemented.
- Strengthen Evaluation Methodologies: Future research should employ rigorous evaluation methods to assess the long-term impact of eye care programs on vision impairment rates and overall eye health outcomes within Indigenous populations. Evaluations should encompass all dimensions of access, including approachability, acceptability, availability, affordability, and appropriateness.
- Address Demand-Side Barriers: While supply-side strategies are important, addressing demand-side barriers is equally crucial. This includes building trust in healthcare services, improving communication and cultural literacy among healthcare providers, and ensuring affordability and accessibility are not just about physical location but also cultural and social accessibility.
Conclusion: Affirming Reality and Embracing Progress
“Is the aboriginal eye care program real?” The answer is unequivocally yes. Significant efforts are underway to address eye health disparities in Indigenous communities through various service delivery models. These programs are making a difference, increasing access to essential eye care services.
However, the journey towards equitable eye health is ongoing. The review reveals critical gaps in geographical and clinical scope, cultural responsiveness, and robust evaluation. Moving forward requires a concerted effort to expand the reach and comprehensiveness of Indigenous eye care programs, deeply embedding cultural sensitivity and community partnership at their core. By prioritizing these areas, we can ensure that eye care services are not only real but truly effective and impactful in improving the lives and vision of Indigenous peoples.