The journey home after a hospital stay is a critical period for patients. Unfortunately, this time is often fraught with challenges. A significant number of patients experience adverse events, such as medication complications or infections, within the weeks following discharge. Alarmingly, a substantial portion of older adults are readmitted to the hospital within just 30 days of being discharged. This cycle of readmissions and adverse events not only impacts patient well-being but also places a considerable strain on healthcare systems.
To address these pressing issues, healthcare institutions are increasingly focusing on transitional care programs. But what is a transitional care program exactly, and why is it so vital? This article delves into the concept of transitional care, exploring its definition, importance, key strategies, and the benefits it offers to both patients and healthcare providers, particularly within the context of neurological conditions.
Defining Transitional Care Programs: Bridging the Gap in Healthcare
Transitional care programs are specifically designed interventions aimed at ensuring a smooth and safe transition for patients as they move between different healthcare settings and providers. This often involves the crucial period when a patient is discharged from a hospital and returns home or moves to another care facility. In essence, these programs act as a bridge, filling the gaps in care coordination that can occur during these transitions.
What is Transitional Care?
Transitional care itself refers to the coordinated set of actions designed to ensure the continued and safe care of patients as they transfer between different locations or levels of care within the healthcare system. This could be a move from:
- Hospital to Home: The most common transition, and often the focus of transitional care programs.
- Hospital to Rehabilitation Facility: For patients requiring ongoing therapy after acute illness or injury.
- Hospital to Skilled Nursing Facility: For patients needing continued nursing care and support.
- Specialist to Primary Care Physician: Ensuring seamless follow-up and ongoing management.
The core goal of transitional care is to prevent disruptions in care, reduce the risk of adverse events, and ultimately improve patient outcomes during these vulnerable transition periods.
Why are Transitional Care Programs Necessary? Addressing Readmissions and Adverse Events
The necessity for transitional care programs stems from the significant challenges patients face after hospital discharge. Several factors contribute to the increased risk during this period:
- Increased Vulnerability: Patients are often still recovering and may be physically weaker or cognitively impaired after a hospital stay.
- Complex Care Regimens: Discharge often involves new medications, therapies, and follow-up appointments, which can be confusing and overwhelming for patients and caregivers.
- Communication Gaps: Information may not be effectively communicated between hospital staff, patients, families, and outpatient providers, leading to misunderstandings and errors.
- Lack of Support at Home: Patients may lack adequate social support, resources, or understanding at home to manage their recovery effectively.
These challenges can lead to a range of negative outcomes, including:
- Adverse Drug Events (ADEs): Medication errors, side effects, and lack of adherence are common post-discharge.
- Hospital-Acquired Infections: Infections developed in the hospital can sometimes manifest or worsen after discharge.
- Worsening of Underlying Conditions: Chronic conditions may not be effectively managed in the transition, leading to relapse or complications.
- Unnecessary Readmissions: Preventable issues arising post-discharge often result in patients needing to be readmitted to the hospital.
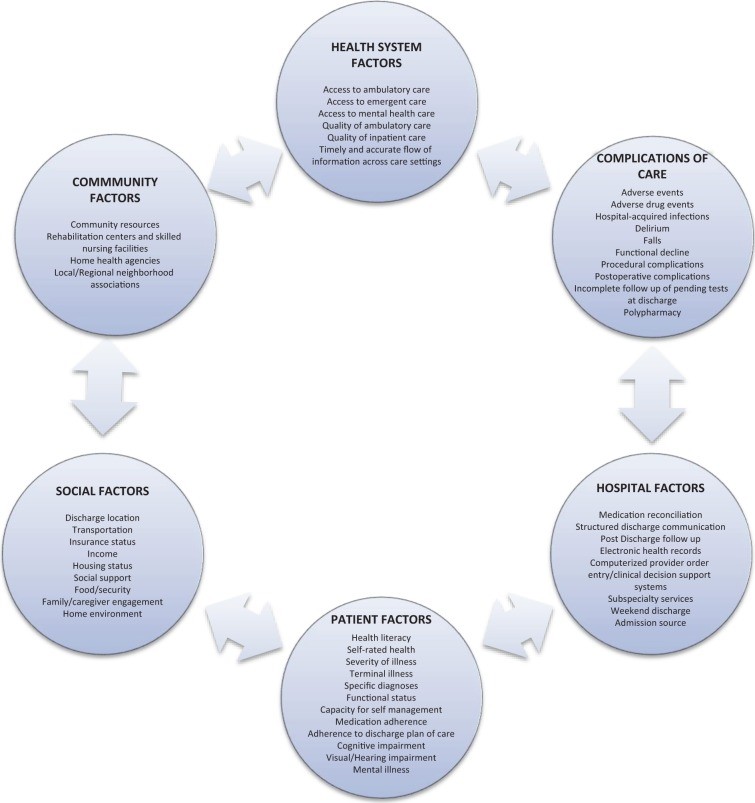
Alt text: Diagram illustrating factors contributing to hospital readmission, including clinical factors, patient-related factors, and healthcare system factors.
Hospital readmissions are a particularly concerning outcome, both for patient well-being and healthcare costs. Readmission rates are used as a key indicator of hospital performance, and in many countries, including the United States, hospitals face financial penalties for high readmission rates, especially for conditions like pneumonia, heart failure, and myocardial infarction. While neurological conditions like stroke may soon be included in these measures, the imperative to improve transitional care for all patients is clear.
Key Components of Effective Transitional Care Programs
While specific program designs vary, effective transitional care programs often incorporate several common elements:
- Predischarge Planning: Starting the transition process while the patient is still in the hospital is crucial. This includes assessing patient needs, providing education, medication reconciliation, and scheduling follow-up appointments.
- Postdischarge Follow-up: Continued support and monitoring after discharge are essential. This can involve phone calls, home visits, or telehealth consultations to check on patient progress, address concerns, and reinforce discharge instructions.
- Dedicated Transition Provider: Having a designated healthcare professional, such as a nurse, case manager, or pharmacist, to oversee the transition process provides a consistent point of contact and ensures coordinated care. This “transition coach” can build rapport with the patient, provide personalized support, and proactively address potential issues.
- Patient and Caregiver Engagement: Empowering patients and their caregivers to actively participate in their care is paramount. This involves providing clear and understandable information, teaching self-management skills, and encouraging them to ask questions and seek help when needed.
- Medication Management: Medication reconciliation (ensuring an accurate and complete list of medications), patient education on medications, and post-discharge medication review are vital to prevent ADEs.
- Communication and Coordination: Facilitating clear and timely communication between hospital staff, patients, families, outpatient providers, and other relevant healthcare professionals ensures everyone is on the same page and reduces the risk of miscommunication.
- “Bridging” Interventions: The most successful programs utilize “bridging” strategies, which combine both predischarge and postdischarge interventions. This continuous support across the transition period is more effective than interventions focused solely on one phase.
The Risk Landscape: Identifying Patients Who Benefit Most from Transitional Care
While all patients benefit from good care transitions, certain populations are at a higher risk of adverse events and readmissions and therefore stand to gain significantly from targeted transitional care programs. These high-risk groups include:
High-Risk Patient Groups
- Older Adults: Aging is often associated with increased frailty, multiple chronic conditions, and cognitive decline, making transitions more challenging.
- Patients with Chronic Illnesses: Individuals with conditions like heart failure, COPD, diabetes, and neurological disorders often require complex care and are more vulnerable to exacerbations post-discharge.
- Neurological Patients: Patients with stroke, epilepsy, multiple sclerosis, and other neurological conditions often face unique challenges related to physical and cognitive impairments, making effective transitions particularly critical.
- Patients with Stroke: Stroke survivors are at high risk of recurrent strokes and other complications, necessitating robust transitional care to manage risk factors and support rehabilitation.
- Patients with Complex Medical Needs: Individuals with multiple comorbidities, polypharmacy (taking many medications), or complex social situations require more intensive support during transitions.
Factors Contributing to Readmission Risk
Beyond specific patient groups, several factors can increase an individual’s risk of readmission and highlight the need for tailored transitional care:
- Poor Functional Status at Discharge: Patients with limited mobility or ability to perform daily activities are more vulnerable at home.
- Advanced Age: Older age is an independent risk factor for readmission.
- Psychiatric Illness: Mental health conditions can complicate recovery and increase readmission risk.
- Limited Access to Social Support: Lack of family or community support can hinder a patient’s ability to manage their health at home.
- Low Socioeconomic Status: Financial constraints and limited access to resources can negatively impact health outcomes post-discharge.
- Lack of Timely Follow-up: Delays in seeing outpatient providers or accessing necessary services can lead to complications.
- Inadequate Discharge Instructions: Unclear or incomplete instructions can lead to patient confusion and errors in self-care.
Successful Transitional Care Strategies: Examples and Effectiveness
Numerous transitional care models and programs have been developed and studied, demonstrating varying degrees of success in reducing readmissions and improving patient outcomes. Here are some prominent examples:
Care Transitions Intervention (CTI)
The Care Transitions Intervention (CTI), developed by Dr. Eric Coleman, is a widely recognized multicomponent program focused on empowering patients to become active self-managers. Key elements of CTI include:
- Patient Engagement and Self-Management Skills: Patients are taught skills to manage their medications, create and use a personal health record, schedule follow-up appointments, and recognize “red flags” indicating worsening conditions.
- Transition Coach: An advanced practice nurse acts as a “transition coach,” providing home visits and phone calls to reinforce self-management strategies and address patient concerns.
- Four Pillars of Care: CTI focuses on medication management, personal health record utilization, primary care follow-up, and recognizing warning signs.
Studies of CTI have shown significant reductions in 30-day readmission rates across various healthcare settings and patient populations, including older adults with stroke and chronic illnesses.
Transitional Care Model (TCM)
The Transitional Care Model (TCM), pioneered by Dr. Mary Naylor, is a nurse-led program specifically designed for chronically ill, high-risk older adults. TCM emphasizes:
- Nurse-Led Care Coordination: A transitional care nurse (TCN) follows patients from the hospital to home, acting as a central coordinator.
- Home Visits and Telephone Follow-up: TCNs conduct home visits and provide ongoing telephone support to monitor patient progress, address needs, and facilitate communication.
- Multidisciplinary Approach: TCNs collaborate with physicians, nurses, social workers, and other healthcare professionals to ensure comprehensive care.
Research on TCM has demonstrated significant reductions in readmission rates at 60 and 90 days, particularly for geriatric patients and those with conditions like heart failure.
Project Re-Engineered Discharge (RED)
Project RED, developed at Boston University Medical Center, is a team-based program focused on improving the discharge process within the hospital setting. Key components of Project RED include:
- Nurse Discharge Advocate (DA): A DA works with patients during their hospitalization to provide education, create a personalized post-discharge plan, and ensure they understand their medications and follow-up care.
- Pharmacist Follow-up: A pharmacist conducts post-discharge phone calls to review medications, address medication-related questions, and communicate with the patient’s primary care provider.
- Multidisciplinary Team Approach: Project RED involves a team of nurses, pharmacists, and other healthcare professionals to optimize the discharge process.
Studies of Project RED have shown reductions in hospital utilization, including both readmissions and emergency department visits.
Project Better Outcomes for Older Adults Through Safe Transitions (BOOST)
Project BOOST, supported by the Society of Hospital Medicine, is a quality improvement initiative designed to help hospitals implement effective transitional care programs. BOOST provides:
- Mentorship and Toolkit: Hospitals implementing BOOST receive guidance from expert mentors and access a toolkit of resources, including risk assessment tools, medication reconciliation protocols, and discharge checklists.
- Quality Improvement Focus: BOOST emphasizes a systematic approach to improving transitional care processes within individual hospitals.
- Multidisciplinary Team Implementation: BOOST encourages hospitals to create multidisciplinary teams to lead and implement their transitional care programs.
Hospitals participating in Project BOOST have demonstrated reductions in 30-day readmission rates, highlighting the effectiveness of a structured quality improvement approach.
Strategies for Neurological Patients: Addressing Specific Needs
While the general transitional care programs mentioned above are beneficial, neurological patients often require tailored strategies to address their unique needs. These may include:
- Secondary Stroke Prevention: For stroke patients, ensuring adherence to medications for blood pressure control, cholesterol management, and antithrombotic therapy is crucial to prevent recurrent strokes.
- Dysphagia Screening and Management: Patients with swallowing difficulties (dysphagia) after stroke or other neurological conditions require specialized dietary modifications and therapy to prevent aspiration pneumonia and ensure adequate nutrition.
- Rehabilitation and Therapy Coordination: Connecting patients with appropriate rehabilitation services (physical therapy, occupational therapy, speech therapy) post-discharge is essential to maximize functional recovery.
- Home Care and Monitoring Protocols: For certain neurological conditions, home care services and remote monitoring technologies can help track symptoms, medication adherence, and overall well-being.
- Symptom Management Protocols: Neurological conditions can cause a range of symptoms (pain, fatigue, spasticity, etc.) that require ongoing management and support post-discharge.
Alt text: Table outlining a taxonomy of interventions to improve transitional care at hospital discharge, categorized into predischarge interventions, postdischarge interventions, and bridging interventions.
Implementing Transitional Care Programs: Key Considerations and Recommendations
Implementing effective transitional care programs requires careful planning and attention to various factors.
Common Features of Effective Programs
Despite the diversity in program design, successful transitional care initiatives share several common characteristics:
- Bridging Interventions: Combining predischarge and postdischarge components for continuous support.
- Dedicated Transition Provider: A designated individual to lead care coordination and patient support.
- Patient Engagement and Empowerment: Actively involving patients and caregivers in the process.
- Focus on Communication: Ensuring clear and timely information exchange among all stakeholders.
- Multidisciplinary Approach: Involving a team of healthcare professionals to address diverse patient needs.
Implementation Challenges
Despite the proven benefits, implementing and sustaining transitional care programs can present challenges:
- Resource Intensive: Effective programs often require dedicated staff, time, and financial investment.
- Cost Justification: Demonstrating the return on investment (ROI) of transitional care programs, particularly in terms of reduced readmissions and cost savings, is crucial for securing funding and support.
- Sustainability: Ensuring long-term program sustainability requires ongoing commitment from hospital leadership and integration into routine care processes.
- Data Collection and Evaluation: Tracking program outcomes, such as readmission rates and patient satisfaction, is essential for demonstrating effectiveness and identifying areas for improvement.
Recommendations for Hospitals and Neurohospitalists
For hospitals and neurohospitalists seeking to enhance transitional care, several recommendations emerge:
- Data-Driven Approach: Start by analyzing hospital-specific readmission data, identifying high-risk patient populations and conditions.
- Interdisciplinary Team Formation: Create a team of physicians, nurses, pharmacists, social workers, and other relevant professionals to design and implement the program.
- Leverage Quality Improvement Infrastructure: Utilize existing quality improvement frameworks and electronic health record systems to support program implementation and data tracking.
- Focus on Key Program Elements: Incorporate core components such as patient engagement, dedicated transition providers, medication reconciliation, communication facilitation, and post-discharge outreach.
- Tailor to Specific Patient Needs: Adapt programs to address the unique needs of specific patient populations, such as neurological patients, by including disease-specific interventions.
- Measure Outcomes and Continuously Improve: Regularly monitor program outcomes, collect feedback, and make adjustments to optimize effectiveness.
Alt text: Table summarizing recommendations for neurohospitalists to improve transitional care, including data collection, team building, and implementation of bundled strategies.
Conclusion: Investing in Transitional Care for a Healthier Future
Transitional care programs are not merely a trend; they are a fundamental necessity for improving patient safety, enhancing recovery, and optimizing healthcare outcomes. By proactively addressing the challenges of care transitions, hospitals and healthcare providers can significantly reduce readmission rates, prevent adverse events, and improve the overall patient experience. For neurohospitalists and institutions caring for neurological patients, implementing robust transitional care programs is particularly crucial to support the complex needs of this vulnerable population and ensure they receive the comprehensive care they deserve throughout their journey to recovery. Investing in transitional care is an investment in a healthier and more efficient healthcare system for all.