Falls are a significant health concern for older adults, but it’s crucial to understand that they are not an inevitable part of aging. A proactive approach with a dedicated Fall Prevention Program In Home Care can significantly reduce risks and enhance the quality of life for seniors. This article will explore the essential aspects of such programs and how they can help your loved ones remain safe and independent in the comfort of their own homes.
Understanding the Importance of Home-Based Fall Prevention
Home is where most falls occur, with a staggering 75% of falls happening within the familiar surroundings of one’s residence. This statistic underscores the critical need for effective fall prevention programs specifically designed for the home environment. These programs go beyond general advice; they offer tailored strategies and expert support right where it’s needed most.
Key Components of a Home Care Fall Prevention Program
A comprehensive fall prevention program in home care integrates several crucial elements to address the multifaceted nature of fall risks:
- Evidence-Based Practices: The most effective programs are rooted in scientific research and clinical best practices, ensuring that care strategies are proven and of the highest quality.
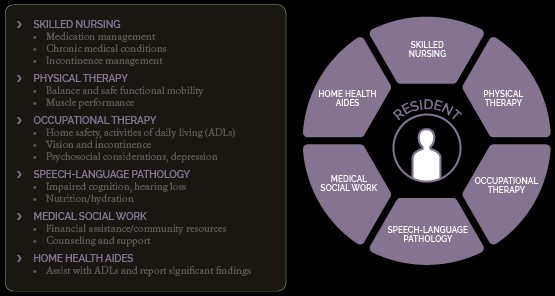
- Interdisciplinary Approach: A diverse team of healthcare professionals, potentially including physical therapists, occupational therapists, nurses, and geriatric specialists, collaborates to assess and address individual risk factors comprehensively. This team approach ensures all aspects contributing to fall risk are considered.
- Expert Care at Home: Receiving care in the home environment is paramount. It allows professionals to identify and mitigate specific hazards within the actual living space, leading to more effective interventions.
- Patient Empowerment: Engaging the individual and their family in the prevention process is key. Programs that encourage active participation and education lead to better long-term outcomes and a greater sense of control.
- Fall Detection Technology: Some programs offer fall detection systems, often for a limited trial period. These systems provide an added layer of safety and peace of mind, alerting caregivers in case of a fall, especially for those living alone.
- Expert Program Development: Collaboration with recognized experts in geriatric fall prevention, like Michelle Lusardi, PT, DPT, PhD, FAPTA (as mentioned in the original article), ensures the program is built on the latest knowledge and best practices in the field.
How Home Health Care Addresses Fall Hazards
Home health care plays a vital role in fall prevention by directly addressing a wide spectrum of potential hazards present in the home. These hazards can be categorized into several key areas:
Musculoskeletal Issues
Problems affecting muscles, joints, nerves, and bones are significant contributors to falls. Home health professionals can assess and treat issues like weakness, pain, and mobility limitations through targeted therapies.
Visual Disturbances
Vision impairments such as cataracts, glaucoma, and macular degeneration can drastically increase fall risk. Home care can help individuals adapt to visual changes and implement strategies to navigate their homes safely despite these challenges.
Functional and Cognitive Impairments
Conditions like memory loss, difficulty with mobility, and impaired problem-solving skills significantly elevate fall risk. Home care programs incorporate cognitive and functional assessments and interventions to support safer living.
Chronic Conditions
Chronic illnesses like Parkinson’s disease, diabetes, dementia, and heart conditions often affect balance and coordination. Home health care provides tailored strategies to manage these conditions and minimize their impact on fall risk.
Medication Management
Certain medications, including sleep aids and some blood pressure medications, can cause dizziness or unsteadiness. Medication review and management are crucial components of home-based fall prevention, ensuring medications are not inadvertently increasing fall risk.
Home Safety Modifications
Identifying and removing hazards within the home is a fundamental aspect of fall prevention. Home health professionals can assess the home environment and recommend modifications such as decluttering, removing throw rugs, securing electrical cords, and improving lighting.
Goals of a Fall Prevention Program
The overarching goals of a fall prevention program in home care are to empower individuals to:
- Understand Their Fall Risk: Comprehensive assessments help individuals and their families understand their specific risk factors.
- Learn Healthy Self-Care Strategies: Education on exercises, safe movement techniques, and healthy habits promotes self-management and reduces dependence on others.
- Improve Quality of Life: By reducing the fear of falling and increasing confidence in mobility, these programs significantly enhance overall well-being and quality of life.
- Avoid Preventable Falls: The primary aim is to proactively prevent falls through targeted interventions and risk factor modification.
- Remain Safely at Home with Independence: Fall prevention programs are crucial for enabling seniors to maintain their independence and continue living in their homes for as long as possible.
- Reduce Expensive Hospitalizations: Preventing falls directly reduces the likelihood of fall-related injuries and costly hospitalizations, benefiting both individuals and the healthcare system.
It’s important to remember that a significant proportion of falls – as high as two-thirds** – are preventable through evidence-based interventions.
Is a Home-Based Fall Prevention Program Right for You?
Consider a fall prevention program in home care if you or your loved one:
- Has experienced a fall within the past year.
- Feels unsteady when standing or walking.
- Expresses worry or fear about falling.
Even seemingly minor incidents like tripping or slipping, or struggling to get up from a chair or bed, can indicate an increased fall risk.
Understanding the Consequences of Falls
Falls are not just accidents; they are the leading cause of injury and death from injury among older adults aged 65 and older. The repercussions of a fall extend far beyond physical injuries.
Falls can trigger a cascade of negative consequences, including a significant fear of falling. This fear can lead to reduced physical activity, resulting in decreased balance and muscle strength, paradoxically increasing the actual risk of future falls. This creates a cycle of fear and decline that a fall prevention program aims to break.
Common Risk Factors for Falls
Identifying risk factors is the first step in effective fall prevention. These factors are broadly categorized as extrinsic (external) and intrinsic (internal).
Extrinsic Risk Factors:
- Home Hazards: Poor lighting, clutter, trip hazards, and uneven surfaces within the home.
- Lack of Exercise: Reduced strength, balance, and coordination due to inactivity.
- Inadequate Home Features: Lack of stair handrails or bathroom grab bars.
- Poor Lighting: Insufficient illumination making navigation difficult.
- Slippery Surfaces: Wet floors or rugs that are not securely fastened.
- Medications: Psychoactive drugs or medications causing dizziness.
- Improper Assistive Device Use: Incorrect use of canes or walkers.
- Inappropriate Footwear: High heels or backless shoes.
Intrinsic Risk Factors:
- Advanced Age: Simply getting older increases risk.
- History of Falls: Previous falls are a strong predictor of future falls.
- Muscle Weakness: Loss of strength, particularly in legs and core.
- Balance and Gait Problems: Difficulties with balance and walking steadily.
- Sensory Impairments: Poor vision or hearing.
- Postural Hypotension: Blood pressure drops upon standing, causing dizziness.
- Low Vitamin D Levels: Vitamin D deficiency can affect muscle strength and balance.
- Foot Pain: Foot problems impacting gait and balance.
- Medical Conditions: Conditions like heart failure, COPD, stroke, diabetes, Parkinson’s, and dementia.
- Fear of Falling: As mentioned, the fear itself can be a risk factor.
The more risk factors present, the higher the likelihood of falls. Home health care services, including occupational and physical therapy, are instrumental in minimizing these risks.
When to Consult Your Doctor
It’s crucial to discuss fall concerns with your doctor if you:
- Have fallen in the past year, even without injury, as this significantly increases future fall risk.
- Use an assistive device like a cane or walker.
- Feel unsteady while walking or standing.
- Need to use your arms to push yourself up from a chair.
- Hold onto furniture for balance when walking at home.
- Take medications that cause dizziness, lightheadedness, or fatigue.
Taking Proactive Steps to Prevent Falls
Preventing falls is possible and highly beneficial. Discuss the Amedisys Fall Prevention Program with your doctor to determine if it’s the right step to ensure safety and independence at home. Your doctor can assess your eligibility for the Medicare Home Health Benefit and initiate the program.