The modern healthcare landscape is characterized by intricate processes, an overwhelming influx of data, and increasingly complex patient needs. This often leads to inefficient workflows that negatively impact patients, caregivers, clinicians, and healthcare staff alike. However, the widespread adoption of health information technology (IT) and advancements in computing offer a significant opportunity to revolutionize healthcare workflows through automation. By strategically implementing automated care programs, healthcare organizations can unlock unprecedented levels of efficiency, enhance the quality of care, and ultimately improve patient outcomes.
Automation, defined as the use of technology to monitor and control the delivery of products and services, is not a novel concept across industries. From manufacturing to finance, automation has transformed operations, boosting productivity and streamlining processes. However, its integration within healthcare has lagged behind, often merely digitizing outdated paper-based workflows rather than fundamentally rethinking and optimizing care delivery. This approach contributes to clinician burnout and prevents the healthcare sector from fully leveraging technology to its advantage. Inefficient workflows are a pervasive issue, contributing to clinician fatigue and burdening patients and caregivers with complex care management responsibilities.
Implementing automated care programs is not simply about adopting new technologies; it’s about strategically redesigning healthcare workflows to maximize efficiency, safety, and patient-centeredness. This article will explore the critical considerations, strategic priorities, and supporting strategies that highlight why implementing an automated care program will significantly improve care delivery, creating a more effective, efficient, and ultimately, a better healthcare experience for everyone involved.
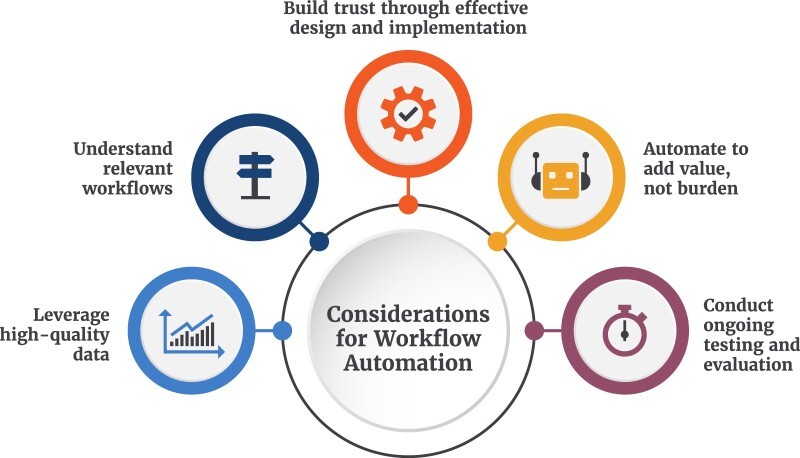
Key Considerations for Successful Automated Care Programs
Successfully integrating automation into healthcare workflows requires careful planning and a deep understanding of the specific needs and challenges within the healthcare ecosystem. Several key considerations are crucial for ensuring that automated care programs are not only implemented but also deliver the intended benefits and improve care delivery.
Leveraging High-Quality Data for Automation
One of the most fundamental prerequisites for effective automation in healthcare is access to high-quality data. The success of any automated care program hinges on the reliability, accuracy, and completeness of the data it utilizes. Poor data quality can lead to inaccurate insights, flawed decision-making, and ultimately, compromised patient care. The data powering automation solutions can encompass a wide spectrum, including administrative details, cost metrics, frequency of procedures, treatment durations, clinical information, and patient outcome data.
Understanding the inherent limitations of data is equally critical. Potential issues such as data incompleteness, inconsistencies across systems, and inaccuracies can undermine the effectiveness of automation. To mitigate these risks, the adoption of industry consensus standards for data collection, storage, and exchange is paramount. These standards ensure data uniformity and interoperability, facilitating seamless data flow and enhancing the reliability of automated tasks. When coupled with evidence-based workflows, standardized data significantly reduces the need for manual data mapping, improves the repeatability of automated processes, and promotes the widespread reuse of successful automation strategies.
 Considerations for advancing health care workflow automation
Considerations for advancing health care workflow automation
Understanding and Optimizing Relevant Workflows
Introducing automation inevitably brings about change. Whether it involves automating a single task or an entire healthcare workflow, the way work is performed will be transformed. Therefore, a thorough understanding of existing workflows and their intended objectives is essential for developing effective automation solutions and accurately measuring their impact. Prior to implementing any automated care program, a comprehensive evaluation of the workflow under consideration is necessary. This includes analyzing the individual tasks or steps involved, the technologies currently in use, the organizational context, and the roles of all individuals participating in the workflow. By meticulously mapping out the current state, healthcare organizations can identify areas ripe for automation and design solutions that seamlessly integrate into the existing operational framework, optimizing workflow design for maximum efficiency.
Building Trust and Ensuring User Buy-in
Gaining the trust and securing buy-in from all relevant stakeholders is absolutely vital for the successful design and implementation of automated care solutions. For automated care programs to be effectively adopted and utilized, those most impacted – patients, caregivers, clinicians, and staff – must be actively involved and invested in the change process. A robust, systematic approach that fully engages stakeholders, including direct users like patients and clinicians, as well as organizational leadership, is crucial for identifying automation needs and clearly defining the anticipated benefits.
Transparent and effective communication is paramount. Establishing clear, shared goals and explaining precisely what the automation aims to improve, how it is expected to function, and what tasks it will and will not replace is essential for building confidence. Conversely, poor communication and negative user experiences, often stemming from inadequate training, can quickly erode trust. If the intended improvements of automation are overshadowed by user frustration and diminished enthusiasm for change, the overall initiative can be jeopardized. This underscores the critical importance of ensuring that automated care solutions are accurate, reliable, user-friendly, and, above all, do not introduce new risks, especially to patient safety.
Automation as a Value-Adding Tool, Not a Burden
The primary driver for introducing automation into healthcare workflows should be a steadfast commitment to delivering high-quality, equitable care. When considering automation, a key factor is whether its implementation will genuinely add value, enhance safety, and improve efficiency. This encompasses ensuring that automation serves all patient populations fairly and does not inadvertently create biases or favor specific demographic groups.
Furthermore, the pursuit of automation often presents valuable opportunities to completely redesign workflows. Instead of simply automating existing inefficient processes, healthcare organizations can leverage automation as a catalyst to re-envision and streamline workflows from the ground up. This holistic approach ensures that automation is not merely a technological add-on but an integral part of a fundamentally improved and more efficient care delivery system.
Continuous Testing, Evaluation, and Improvement
Testing and evaluation are not one-time events but ongoing processes that must be conducted before, during, and after the implementation of any automated care program. Effective automation initiatives incorporate feedback loops that enable continuous monitoring of both the automation technology itself and its broader impact on workflows and outcomes. This continuous assessment is crucial for verifying whether the automation is functioning as intended, measuring its actual impact on key performance indicators, and determining if it is indeed leading to tangible improvements and achieving the defined automation goals.
Ultimately, the implementation of automation must translate into measurable improvements across one or more dimensions of the healthcare delivery ecosystem. Therefore, all automation efforts must be carefully designed to track and quantify these improvements, providing concrete evidence of the value and effectiveness of the automated care program.
These considerations provide a solid foundation for advancing workflow automation in healthcare, paving the way for the development and implementation of well-defined priorities and effective strategies.
Strategic Priorities for Implementing Automated Care Programs
Building upon these key considerations, a set of strategic priorities is essential to guide the successful implementation of automated care programs and drive meaningful improvements in care delivery. These priorities address the diverse ecosystem of healthcare organizations and stakeholders, including patients, caregivers, clinicians, staff, and the technologies that collectively support advancements in healthcare workflow automation. They serve as a roadmap for both near-term actions to initiate automation and long-term planning to achieve a fully optimized and automated healthcare environment.
Priority 1: Nationwide Scalable Automation – Sprints and Marathons
Transforming healthcare through automation requires a dual approach, balancing immediate, achievable gains with long-term, transformative initiatives. Adopting workflow automation should be viewed as a journey with iterative phases, progressing towards a desired future state. This involves implementing “sprints” – smaller, feasible automation projects that deliver rapid, tangible benefits and foster buy-in within the healthcare community. These early successes pave the way for “marathons” – more ambitious, long-term automation efforts aimed at completely automating entire processes. Leveraging technologies that can seamlessly integrate into diverse electronic ecosystems, regardless of an organization’s size or technological sophistication, is crucial for achieving scalable automation. The informatics community plays a vital role in developing tools and methodologies, such as natural language processing and machine learning, to support this priority. Further informatics research is needed to rigorously identify workflows that are prime candidates for automation and to build a robust evidence base for implementing broader automation solutions at scale.
Priority 2: Identifying and Eliminating Redundant Tasks
Unlocking the full potential of automation in healthcare requires a systematic approach to identifying and eliminating redundant tasks. This involves thoroughly analyzing the infrastructure, processes, and systems used by healthcare organizations to pinpoint tasks that are unnecessarily duplicated across different staff roles and operational areas. Employing established workflow analysis techniques and conducting comprehensive technological assessments of existing infrastructure and resources are essential steps in creating a detailed inventory of redundant tasks and evaluating their readiness and complexity for automation. Informatics approaches and tools that can leverage data from health IT systems and are easily deployable across diverse healthcare organizations are needed to facilitate the identification of these redundant workflows. Research and demonstration projects focused on developing and validating such approaches and tools are crucial to demonstrate their effectiveness and scalability.
Priority 3: Preparing Clinicians for Workflow Automation
Clinicians today navigate a complex landscape of new technologies, evolving regulatory mandates, and shifting business priorities, all while striving to provide the best possible care for their patients. Technology changes can understandably be perceived as adding to existing burdens and raising concerns, particularly regarding patient safety. Therefore, successful workflow automation initiatives must actively involve clinicians throughout the entire process to foster acceptance and address concerns. Informatics methods and research focused on the human-centered design and seamless implementation of health IT are paramount to advancing workflow automation in a clinician-friendly manner. Ensuring a ready clinician base that embraces automation is key to realizing its full potential.
Priority 4: Empowering Stakeholders for Effective Engagement
Healthcare has witnessed remarkable technological advancements in diagnosis, treatment, and self-management. The widespread adoption of health IT has further empowered clinicians, staff, patients, and caregivers with access to expanded health information and care-related digital functionalities. Automation solutions should build upon the lessons learned from health IT implementation, aiming to eliminate redundancy and streamline tasks for healthcare professionals, patients, and caregivers alike. The informatics research community can significantly contribute by developing and rigorously testing automation solutions that effectively reduce administrative burden for all stakeholders, fostering effective stakeholder engagement in health and healthcare tasks.
Priority 5: Enhancing Patient and Caregiver Interactions
Patients and caregivers often encounter a labyrinthine network of healthcare services and interactions, demanding active care and information management while simultaneously juggling care coordination and information sharing with providers, payers, employers, and other involved parties. The design and implementation of workflow automation solutions should prioritize improving the overall patient and caregiver experience, simplifying care management, and providing robust support for caregivers. Automation should facilitate seamless access to healthcare services and health data, streamline administrative tasks such as appointment scheduling and portal navigation, and make health and healthcare management significantly less cumbersome. Consumer health informatics research is crucial for both developing innovative solutions and rigorously evaluating their effectiveness in enhancing patient and caregiver interactions.
Priority 6: Leveraging Interoperable Health Data
Interoperable data is the lifeblood of effective workflow automation. While recent progress in health IT has enhanced the interoperable use of health information across the healthcare industry, realizing the full potential of workflow automation necessitates the widespread availability of standardized data, both within individual organizations and across the broader healthcare ecosystem. This data is essential for identifying automation opportunities, defining automation needs, and developing and evaluating potential solutions. The informatics community plays a critical role in continuously improving interoperability by pinpointing data access gaps, defining essential health data standards, and rigorously assessing the availability and suitability of health data for both identifying automation needs and informing the design and evaluation of automated care programs.
Table 1. Health care workflow automation priorities, desired end state, and goals
| Priorities | Desired end state | Goals |
|---|---|---|
| 1. Mobilize nationwide scalable automation in near-term “sprints” and long-term “marathons”. | • The health care industry aligns to pursue automation for widespread gains. | – Identify smaller, feasible automation opportunities that can be implemented rapidly where numerous stakeholders benefit in the near-term. – Plan longer-term efforts that fully automate entire processes. – Use technologies that easily can be plugged into an electronic ecosystem, regardless of the size, type, and sophistication of an organization’s technology. |
| 2. Enable discovery of redundant tasks. | • Organizations independently identify automation opportunities. | – Create an operational routine and culture of identifying workflows to automate across health care organizations. – Promote a workforce with the skills needed to analyze existing workflows and data, design and implement automation, and conduct ongoing monitoring and optimization. – Scale automation initiatives across health care organizations in a manner that supports organizations of different sizes, resources, and patient population. |
| 3. Ensure a ready clinician base for workflow automation. | • Clinicians embrace automation to relieve workflow burden. | – Reinvigorate the joy of practice by designing automation that supports cognitive tasks and patient interaction. – Improve situational awareness for care management by identifying and filling data blind spots to provide person-centered care. – Uphold strict and high levels of data security and patient safety. – Streamline data collection, review, and translation for patient care and population health. |
| 4. Enable all stakeholders to effectively and efficiently engage in health and health care tasks. | • Individuals’ time shifts from repetitive to cognitive tasks of managing and supporting care. | – Simplify redundant data entry at multiple points within and across health care encounters. – Eliminate “hunting and gathering” data across multiple platforms by enabling easy access to information for use in decision making. – Present complete, accurate data for workflows through tools that streamline care management. – Improve feedback and status monitoring across the continuum of care and across settings. |
| 5. Improve patient and caregiver interactions with health and health care. | • Patients and caregivers have a more seamless and integrated experience in health and health care management. | – Streamline information and data sharing across patients, caregivers, clinicians, provider and payor staff, and other stakeholders involved in health care workflows. – Simplify administrative tasks such as appointments, registration, portals, and applications for health data access. – Empower patients to manage health by facilitating faster access to needed information. – Improve care access and outcomes by reducing barriers, allowing care to be managed anytime and anywhere. |
| 6. Leverage interoperable health data for automation. | • Data shared across disparate technologies deliver insights and efficiencies. | – Streamline health information exchange workflows. – Improve situational awareness for care management by finding, parsing, and presenting data across multiple systems. – Reduce use of paper forms and processes that require multiple inputs of clinical and administrative information. – Integrate clinician and patient workflows by bringing information, communication, and care into harmony. |
Supporting Strategies for Successful Automation Adoption
To effectively advance these priorities and realize the transformative potential of automated care programs, a set of interconnected supporting strategies is essential. These strategies are designed to work synergistically, fostering a conducive environment for the widespread adoption and successful implementation of workflow automation across the healthcare landscape.
Educate, Convene, Prioritize, Demonstrate, Incent, Scale
Six key strategies underpin the advancement of healthcare workflow automation priorities:
- Educate: Raising awareness is the first crucial step. This involves educating all stakeholders about the pressing need for automation in healthcare, highlighting the immense opportunities it presents, and proactively addressing any perceived barriers to adoption. Comprehensive education initiatives can dispel misconceptions, build enthusiasm, and foster a shared understanding of the benefits of automated care programs.
- Convene: Building a national dialogue is essential for collaborative progress. Creating platforms for multi-stakeholder conversations focused on advancing workflow automation priorities is crucial. These dialogues should bring together patients, caregivers, clinicians, health IT developers, payers, policymakers, and researchers to foster shared understanding, identify common goals, and forge collaborative pathways forward.
- Prioritize: Strategic prioritization is key to effective resource allocation. A systematic process for identifying and prioritizing specific workflows that are most suitable for automation is necessary. This prioritization should consider factors such as potential impact on patient care, feasibility of automation, and alignment with organizational goals. Furthermore, determining the appropriate level of automation for each workflow is crucial to optimize resource utilization and maximize impact.
- Demonstrate: Rigorous testing and evaluation are essential to validate the effectiveness of automation approaches. Pilot projects and demonstration initiatives are needed to test and evaluate various automation strategies in real-world healthcare settings. These demonstrations provide valuable insights into the practical implementation challenges and benefits of different automation solutions, building confidence and informing wider adoption.
- Incent: Policy and market mechanisms play a vital role in driving adoption. Designing and implementing appropriate policy and market incentives to support workflow automation is crucial. Incentives can encourage healthcare organizations to invest in automation technologies, promote innovation in automation solutions, and reward the successful implementation of automated care programs that deliver tangible improvements in care delivery.
- Scale: Dissemination and widespread adoption are the ultimate goals. Effective automation approaches need to be disseminated and scaled across diverse healthcare organizations and workflows. Sharing best practices, developing implementation guides, and providing technical assistance are essential for facilitating the widespread adoption of successful automation strategies and maximizing their impact on the healthcare system as a whole.
Table 2. Strategies to advance health care workflow automation priorities
| Supporting strategies | Strategy focus |
|---|---|
| Educate | Increase awareness of the need and opportunity to automate, identify, and address barriers to automation. |
| Convene | Build national dialog on advancing priorities for workflow automation with multiple stakeholders. |
| Prioritize | Identify and prioritize workflows for automation and appropriate level of automation. |
| Demonstrate | Test and evaluate automation approaches. |
| Incent | Design and implement needed policy and market levels to support workflow automation. |
| Scale | Disseminate effective automation approaches across health care organizations and workflows. |
Crucially, patients and caregivers must be integral participants in national conversations about workflow automation. Their perspectives and needs are paramount to ensuring that automation solutions are designed and implemented in a patient-centered manner. Similarly, healthcare professionals and organizations must be actively engaged in prioritizing workflows for automation, as well as in the design and implementation processes. The health IT and technology community must play a proactive role in developing and instrumenting technologies that facilitate workflow automation design and evaluation, working in close collaboration with potential users. Researchers are essential to advancing automation priorities through rigorous development and evaluation efforts. Finally, payers, policymakers, and accrediting bodies must create an enabling environment that incentivizes the development, testing, and utilization of automation solutions that demonstrably deliver value to patients, caregivers, healthcare professionals, and the healthcare system as a whole.
Conclusion: Maximizing Automation for 21st Century Healthcare
The six priorities and supporting strategies outlined provide a clear roadmap for advancing the use of automation in healthcare. Based on extensive stakeholder input, literature review, and expert workshops, they articulate a collaborative pathway for leveraging modern technology to enhance efficiency, improve health outcomes, and deliver greater value to patients, caregivers, clinicians, staff, and all stakeholders who contribute to health and healthcare. While some workflows are ripe for near-term automation, offering immediate benefits, others require more extensive long-term planning and development.
Workflows with attributes like manual data entry, repetitive tasks, or high frequency are prime candidates for automation. Administrative workflows related to prior authorization, clinical documentation, and reimbursement, which are known burdens for clinicians and patients, stand to benefit significantly from automation. In treatment and care delivery, automation can enhance medication reconciliation, streamline care transitions, improve data identification, and optimize laboratory results review and communication. For population health management, automation can facilitate the implementation of guideline-based approaches for patient identification and care management protocols. Finally, in reporting workflows, automation can streamline public health reporting and adverse event reporting by automating data extraction, report generation, and submission processes.
Implementing automated care programs represents a fundamental shift in thinking across the entire healthcare ecosystem. It is a call to action to embrace the transformative potential of technology and create new opportunities within healthcare, from clinical care to public health reporting. This shift may necessitate the development of new workforce roles and training programs as healthcare organizations increasingly adopt automation and various automation approaches. Ultimately, the focus of automation must be on enhancing safety, strengthening patient-provider relationships, freeing up valuable time for direct patient care, and generating faster, more insightful data to drive continuous improvement in health and healthcare. By embracing these priorities and strategies, healthcare can fully realize the promise of automated care programs to improve care delivery and build a more effective and patient-centered healthcare system for the 21st century.
REFERENCES
[1] Bodenheimer T, Sinsky C. From triple to quadruple aim: care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6. [ PubMed ]
[2] Sinsky C, Dyrbye LN, West CP, Satele D, Tutty S, Shanafelt TD. Professional satisfaction and burnout in US physicians: a systematic review and meta-analysis. Mayo Clin Proc. 2017 Dec;92(12):1805-1823. [ PMC free article ] [ PubMed ]
[3] Mamykina L, Vawdrey DK, Hripcsak G. Data mining electronic health records to improve the efficiency of clinical trials. Clin Trials. 2011 Dec;8(6):707-16. [ PMC free article ] [ PubMed ]
[4] Murdoch TB, Detsky AS. The inevitable application of big data to health care. JAMA. 2013 Mar 20;309(19):2037-8. [ PubMed ]
[5] Patel RS, Longhurst CA, Harrington RA. Precision medicine 2.0: big data and the quest for tailored therapeutics. JAMA. 2015 Jul 14;314(2):125-6. [ PubMed ]
[6] Carayon P. Handbook of human factors and ergonomics. 4th ed. Boca Raton (FL): CRC Press; 2012. Work system analysis.
[7] Dyrbye LN, Shanafelt TD, Sinsky CA, Cipriano PF, Bhatt J, Ommaya A, West CP, Britnell S, Wang H, Trockel M, Tutty S, Wang L, Carlasare M. Burnout among health professional students: a systematic review and meta-analysis. Acad Med. 2017 Mar;92(3):322-31. [ PubMed ]
[8] West CP, Dyrbye LN, Shanafelt TD. Physician burnout: contributors, consequences and solutions. J Intern Med. 2018 Jun;283(6):516-529. [ PubMed ]
[9] Lluch M. Healthcare professionals’ organizational barriers to health information technologies–a systematic review. Int J Med Inform. 2011 May;80(5):281-95. [ PubMed ]
[10] Cresswell KM, Sheikh A. Organizational issues in the implementation and adoption of health information technology innovations: an interpretative review. Int J Med Inform. 2013 May;82(5):e73-86. [ PubMed ]
[11] Berwick DM, Nolan TW, Whittington J. The triple aim: care, health, and cost. Health Aff (Millwood). 2008 May-Jun;27(3):759-69. [ PubMed ]
[12] Institute of Medicine (US) Committee on the Learning Health Care System in America; Smith M, Saunders R, Stuckhardt L, McGinnis JM, editors. Best care at lower cost: the path to continuously learning health care in America. Washington (DC): National Academies Press (US); 2013 May 10.
[13] McGlynn EA, Asch SM. Developing a clinical performance measurement system. Am J Manag Care. 1998;4(1 Spec No):S21-30. [ PubMed ]
[14] Nelson EC, Splaine M, Batalden PB, Plume SK, Carey TS, Davidoff F. Building a science of health care improvement. Ann Intern Med. 2008 Sep 16;149(7):483-8. [ PubMed ]
[15] Shanafelt TD, Boone SL, Tan L, Dyrbye LN, Sotile W, Satele D, West CP, Sloan J, Oreskovich MR. Burnout and satisfaction with work-life balance among US physicians relative to the general US population. Arch Intern Med. 2012 Oct 8;172(18):1377-85. [ PubMed ]
[16] Blumenthal D, Tavenner M. The “meaningful use” regulation for electronic health records. N Engl J Med. 2010 Aug 5;363(6):501-4. [ PubMed ]
[17] Jha AK, DesRoches CM, Campbell EG, Donelan K, Rao SR, Ferris TG, Shields AE, Rosenbaum S, Blumenthal D. Use of electronic health records in U.S. hospitals. N Engl J Med. 2009 Apr 16;360(16):1628-38. [ PubMed ]
[18] Dean J. Challenges and opportunities in building intelligent systems [Internet]. Google Research. [cited 2022 Feb 25]. Available from: https://research.google/pubs/pub43150/
[19] LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015 May 28;521(7553):436-44. [ PubMed ]
[20] Parasuraman R, Parasuraman A. Automation and human performance: theory and applications. Boca Raton: CRC press; 2017.
[21] Okubo TH, Kallem C, Samarth A, Kemper N, Zayas-Cabán T. Workflow automation in health care: qualitative key informant interviews on opportunities, barriers, and strategies. J Am Med Inform Assoc. 2022 Feb 15;29(3):443-451. [ PMC free article ] [ PubMed ]
[22] Okubo TH, Kallem C, Samarth A, Kemper N, Zayas-Caban T. Workflow automation in health care: workshop proceedings on opportunities, barriers, and strategies. [cited 2022 Feb 25]. Available from: https://www.healthit.gov/sites/default/files/page/2021-09/WorkflowAutomationWorkshopSummaryReport.pdf
[23] ONC’s mission and vision [Internet]. HealthIT.gov. [cited 2022 Feb 25]. Available from: https://www.healthit.gov/onc/mission
[24] Workflow automation in health care [Internet]. HealthIT.gov. 2020. [cited 2022 Feb 25]. Available from: https://www.healthit.gov/topic/other-hot-topics/workflow-automation-health-care
[25] Office of the National Coordinator for Health Information Technology. Workflow automation in health care workshop [Internet]. 2021. [cited 2022 Feb 25]. Available from: https://www.healthit.gov/sites/default/files/page/2021-07/WorkflowAutomationWorkshopAgenda.pdf
[26] ONC annual meeting [Internet]. HealthIT.gov. [cited 2022 Feb 25]. Available from: https://www.healthit.gov/annualmeeting/agenda
[27] Kahn MG, Callahan TJ, Barnard J, Bauck A, Brown JS, Davidson NO, Evans JP, Grossman MK, Holmes JH, Johnson SG, Liss DT, McCallie D, Mondschein JI, Rosenthal GE, Rowe CA, Ruggeri R, Somkin CP, Stone DJ, Tachinardi U, Waitzman AA, Warnick RE, Williams MS, Wolf SM, Vest JR. A 10 year vision for biomedical informatics: bridging translational research and clinical care. J Am Med Inform Assoc. 2016 Jan;23(1):9-15. [ PMC free article ] [ PubMed ]
[28] Weiskopf NG, Weng C. Methodological approaches for studying the effects of health information technology on patient safety. BMJ Qual Saf. 2013 Feb;22 Suppl 1:i48-53. [ PMC free article ] [ PubMed ]
[29] Jiang X, Finlayson SG, Dave KD, Kale DC, Kohane IS, Palmer NR, Dreyer KJ, Shah NH. Assessing and improving the quality of structured data in electronic health records. J Am Med Inform Assoc. 2017 Mar;24(2):245-251. [ PMC free article ] [ PubMed ]
[30] Dolin RH, Alschuler L, Boyer S, Beebe C, Behlen FM, Biron PV, Shabo R. HL7 Clinical Document Architecture, Release 2. J Am Med Inform Assoc. 2006 Jan-Feb;13(1):30-9. [ PMC free article ] [ PubMed ]
[31] HL7 Fast Healthcare Interoperability Resources (FHIR) [Internet]. HL7 International. [cited 2022 Feb 25]. Available from: https://www.hl7.org/fhir/
[32] Sittig DF, Singh H. A new socio-technical model for studying clinical work in complex adaptive healthcare systems. Qual Saf Health Care. 2010 Oct;19 Suppl 3:i68-74. [ PMC free article ] [ PubMed ]
[33] Holden RJ. What stands in the way of technology-induced patient safety? A conceptual analysis based on normalization process theory. BMJ Qual Saf. 2011 Feb;20 Suppl 1:i37-43. [ PubMed ]
[34] Saleem JJ, Bangerter AK, Ruijter A,জমেন্ট, and care delivery workflows as these are all areas that require greater data exchange and place higher cognitive loads on clinicians and burden patients and caregivers as a result. Automation has the potential to assist clinicians in identifying patient data from an external network transaction (eg, from health information networks) and aid with patient communication, by automatically generating a tailored, patient-specific summary or explanation (eg, for laboratory results). With regards to population health management, automation may aid practices in implementing guidelines-based approaches to identify newly diagnosed patients and recommended care management protocols. Finally, reporting-related workflows associated with state and/or federally mandated public health reporting or adverse event reporting might benefit from automation that can identify relevant requirements, extract needed data, and automatically generate and, upon approval, submit reports on behalf of clinicians, practices, or provider organizations to appropriate registries, agencies, or systems.
Figure 3.
Sample workflows to automate.
The priorities and strategies constitute a call to action to begin that work as part of the direction set by the 21st Century Cures Act.59 Adding automation requires a mind shift across the entire ecosystem, but will help create opportunities across health care from clinical care to public health reporting. This shift may require new workforce, roles, and training as health care implements more automation and different automation approaches.60 It will also require automation of tasks that are focused on ensuring safety, improving patient-provider relationships, providing more time for treatment, and yielding better and faster insights about health and health care.
ONC is creating a health IT ecosystem that will enable automation by advancing the necessary access, exchange, and use of electronic health information through policies and programs.61,62 Through ongoing investment in data standards development and adoption that will help ensure data quality, ONC is facilitating use of those data across multiple systems and applications.63,64 ONC projects may serve as models for pilot testing of health care automation approaches.65 ONC will continue to collaborate with public and private sector stakeholders while it advances policies and technology-related investments to enable workflow automation.
FUNDING
This work was partially funded through U.S. Department of Health and Human Services Contract Number HHSP233201600030I/75P00119F37001, with Clinovations Government + Health, and by the U.S. National Library of Medicine, National Institutes of Health.
AUTHOR CONTRIBUTIONS
TZ-C and THO led the development of the priorities and strategies through a series of coordinated activities which gathered stakeholder input, and SP provided executive leadership and critical appraisal and input to the priorities and strategies. All authors led drafting of the article. All authors revised the article critically, provided intellectual content, and approved the final version for submission. The order of authors listed in the manuscript has been approved by all authors. TZ-C served as Chief Scientist and THO was senior program analyst at the Office of the National Coordinator for Health Information Technology until February 2021 and November 2021, respectively. TZ-C provided executive leadership, and both TZ-C and THO oversaw the overarching project that examined the use of workflow automation in health care.
ACKNOWLEDGEMENTS
The authors thank Spire Communications for copy editing, graphics development support, and reference formatting assistance. We thank the Clinovations Government + Health team—which includes Anita Samarth, Crystal Kallem, and Nicole Kemper—for their leadership and contributions to the overarching project that examined the use of modern computing to advance workflow automation and to the development of the priorities and strategies. Additionally, the authors thank all of the individuals who provided input and expertise into the development of the priorities and strategies.
CONFLICT OF INTEREST STATEMENT
None declared.
Contributor Information
Teresa Zayas-Cabán, National Library of Medicine, National Institutes of Health, Bethesda, Maryland, USA.
Tracy H Okubo, Office of the Chief Information Officer, U.S. Department of Health and Human Services, Washington, District of Columbia, USA.
Steven Posnack, Office of the National Coordinator for Health Information Technology, Washington, District of Columbia, USA.