California has taken a significant step towards overhauling its mental health system, a move that implicitly addresses critical needs within its correctional facilities. Governor Gavin Newsom recently signed Senate Bill 326 (SB 326) and Assembly Bill 531 (AB 531), collectively known as Proposition 1, marking the most substantial reform in decades. While not explicitly focused on prisons, these bills lay the groundwork for establishing and enhancing mental health care programs within these institutions by modernizing the state’s overall behavioral health infrastructure. This legislative package, slated for the March 2024 ballot, promises to channel billions of dollars into revamping mental health services, offering a unique opportunity to address the long-neglected mental health crisis within prisons.
The Imperative for Mental Health Programs in Prisons
The need for robust mental health programs within prisons cannot be overstated. Incarcerated individuals are disproportionately affected by mental health conditions compared to the general population. Factors such as pre-existing conditions, the trauma of incarceration, and the harsh realities of prison life exacerbate mental health issues, leading to a cycle of suffering and recidivism. Addressing these needs is not only a matter of ethical imperative but also crucial for public safety and successful rehabilitation.
Proposition 1, while broad in scope, offers a framework that can be leveraged to improve mental health care within prisons. By modernizing the Mental Health Services Act (MHSA) through SB 326 and allocating $6.38 billion via AB 531, California is setting the stage for a more comprehensive and responsive behavioral health system. This investment is intended to prioritize Californians with the most acute needs, including those experiencing homelessness and substance use disorders. Although prisoners are not explicitly mentioned in the primary target groups, the expansion of services and infrastructure inevitably creates opportunities to extend care to incarcerated populations.
The $6.38 billion bond from AB 531 is particularly noteworthy. It is earmarked for building over 11,150 new behavioral health beds and housing units, alongside 26,700 outpatient treatment slots. This massive capacity increase is designed to touch tens of thousands of lives annually, addressing critical gaps in care across the state. For prisons, this could translate to increased resources and infrastructure for mental health programs, potentially alleviating overcrowding in existing facilities and creating dedicated spaces for treatment and stabilization.
Governor Newsom emphasized the urgency and scope of these reforms: “These reforms, and this new investment in behavioral health housing, will help California make good on promises made decades ago. We see the signs of our broken system every day – too many Californians suffering from mental health needs or substance use disorders and unable to get support or care they need. This will prioritize getting people off the streets, out of tents and into treatment.” While “streets” and “tents” highlight the homeless population, the underlying principle of providing support and care to those in dire need is equally applicable to incarcerated individuals struggling with mental health issues.
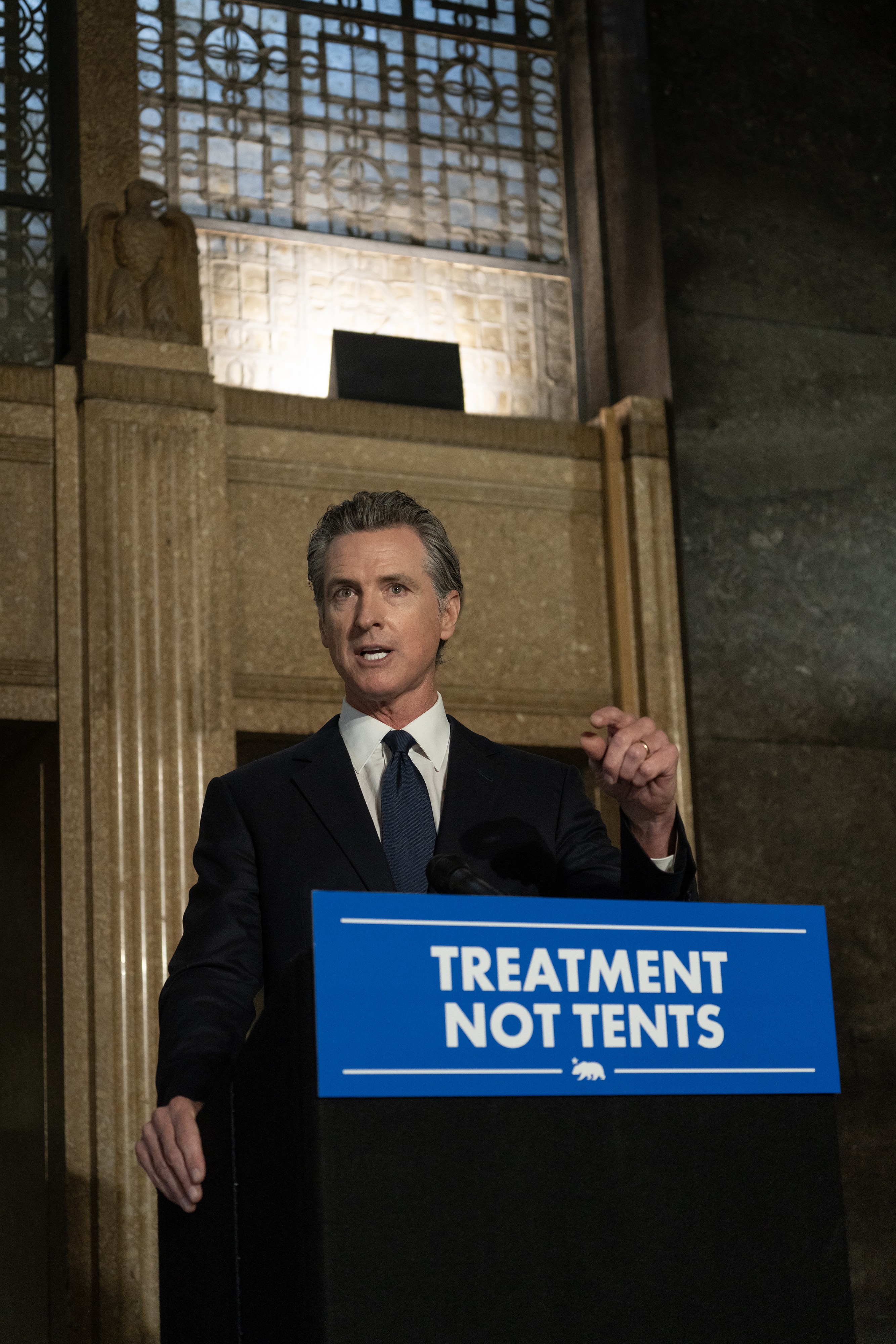 Governor Gavin Newsom signing Senate Bill 326 and Assembly Bill 531, landmark legislation for mental health reform in California.
Governor Gavin Newsom signing Senate Bill 326 and Assembly Bill 531, landmark legislation for mental health reform in California.
Key Components of the Reform and Implications for Prisons
Senate Bill 326 is pivotal in modernizing the MHSA to align with contemporary behavioral health needs. It broadens the scope of services to include substance use disorders, prioritizes care for individuals with severe mental illness, and ensures sustained funding for housing and workforce development. Crucially, it emphasizes accountability and results-oriented outcomes. For prisons, this modernization could mean:
- Expanded Service Eligibility: Including substance use disorders within the MHSA framework is highly relevant to prisons, where substance abuse is often intertwined with mental health issues and criminal behavior.
- Prioritized Care for Severe Mental Illness: This focus directly addresses the significant population within prisons suffering from serious mental illnesses, ensuring they receive the necessary level of care.
- Resource Allocation for Housing and Workforce: While “housing” in the context of prisons may refer to specialized mental health units rather than community housing, the principle of providing appropriate living environments conducive to mental health recovery is applicable. Workforce development can also translate to better training and staffing for mental health professionals working in correctional settings.
Assembly Bill 531’s $6.38 billion bond is the financial engine driving this transformation. It earmarks funds for 11,150 new treatment beds and supportive housing units, as well as outpatient capacity to serve tens of thousands. A dedicated $1 billion is set aside for veterans’ housing, recognizing the specific needs of this population, which is also represented within the prison system. For prisons, AB 531 offers the potential for:
- Infrastructure Development: Funding can be directed towards building or renovating mental health units within prisons, creating therapeutic environments for treatment.
- Enhanced Treatment Capacity: The creation of new treatment beds and outpatient slots can alleviate the strain on existing prison mental health services, allowing for more comprehensive and individualized care.
- Specialized Programs for Veterans: The veteran-specific funding component could inspire or support tailored mental health programs for incarcerated veterans, addressing their unique needs and experiences.
A Statewide Mental Health Movement with Correctional Implications
Governor Newsom’s broader “California Mental Health Movement,” a multi-year plan encompassing over $28 billion, further underscores the state’s commitment to addressing the mental health crisis comprehensively. This movement is built on four pillars:
- Treatment and Housing: A significant $10.9 billion is allocated to create approximately 24,800 beds/units and 45,800 outpatient treatment slots. This massive expansion can indirectly benefit prison systems by increasing the overall availability of mental health services and potentially easing the burden on correctional facilities to provide all levels of care internally.
- Increased Access to Services: Over $10.1 billion is dedicated to expanding access to mental health services for all Californians. While the primary focus is on Medi-Cal and private insurance, the overarching goal of improved access can influence the standard of care expected within all state-run institutions, including prisons.
- Workforce Development: Investing $5.1 billion, with a proposed additional $2.4 billion, to train over 65,000 new health care workers is crucial. This workforce expansion can address the chronic shortage of mental health professionals in all sectors, including corrections, leading to better staffing ratios and specialized expertise within prison mental health programs.
- Support for Kids: While focused on youth mental health, this pillar highlights the state’s commitment to early intervention and prevention. Addressing mental health issues early can have long-term effects, potentially reducing the likelihood of future incarceration and the cycle of mental illness within families that are often impacted by the prison system.
Voices of Support and the Path Forward
The legislative reforms have garnered widespread support from various stakeholders, highlighting the collective recognition of the mental health crisis and the need for systemic change. Senator Susan Talamantes Eggman, author of SB 326, emphasized the need to update the MHSA to address current needs, including substance use disorders, and ensure accountability. Assemblymember Jacqui Irwin, author of AB 531, highlighted the importance of providing housing and treatment services, particularly for vulnerable veterans.
Darrell Steinberg, the original author of the MHSA, acknowledged the progress made over the past two decades but stressed that the work is incomplete. He lauded Governor Newsom’s leadership in prioritizing mental health and substance abuse care, stating that these reforms move the state dramatically closer to fulfilling its promises.
The overwhelming sentiment is that Proposition 1 represents a crucial step forward in transforming California’s behavioral health system. While the immediate focus may be on community-based services and homelessness, the scale and scope of these reforms create a significant opportunity to enhance mental health care programs within prisons. By leveraging the increased funding, expanded service framework, and emphasis on workforce development, California can begin to address the long-standing mental health crisis within its correctional facilities, fostering safer environments, promoting rehabilitation, and ultimately contributing to healthier communities. The passage of Proposition 1 in March 2024 will be a critical moment in realizing this vision and establishing a more humane and effective approach to mental health care for all Californians, including those behind bars.