Palliative care is increasingly recognized as a vital component of comprehensive cancer care. Extensive research highlights the benefits of integrating early palliative care for individuals facing advanced cancer, including improved symptom management, enhanced patient satisfaction, and reduced psychological distress. This evidence has fostered a global consensus advocating for the routine integration of early palliative care into cancer treatment protocols.
Implementation science, the study of methods to integrate research into practice, offers a crucial lens for translating the proven benefits of palliative care into tangible hospital programs. By understanding and addressing the barriers that hinder the adoption of effective interventions, we can bridge the gap between evidence and practice, ensuring patients receive timely and comprehensive care. However, guidance on implementing timely palliative care within cancer services remains limited, and referrals often occur late in the disease trajectory, if at all. Many healthcare leaders responsible for program implementation may lack familiarity with implementation science, hindering real-world progress.
This guide aims to address this gap by providing a practical framework for building a hospital-based palliative care program. It draws upon a systematic review of existing literature to identify key implementation frameworks, enablers, and barriers encountered in integrating palliative care into hospital-based oncology services. By understanding these factors, healthcare professionals and administrators can strategically plan and implement effective palliative care programs, ultimately improving the quality of life for patients with advanced cancer.
Understanding Implementation Science Frameworks in Palliative Care
Implementation science frameworks provide a structured approach to developing, implementing, and evaluating complex interventions like hospital-based palliative care programs. These frameworks offer a roadmap, ensuring systematic consideration of the various factors influencing program success and sustainability. While numerous implementation frameworks exist, this review identified several prominent models utilized in the context of integrated palliative care:
- RE-AIM Framework (Reach, Effectiveness, Adoption, Implementation, Maintenance): This framework emphasizes the broad public health impact of interventions, focusing on five key dimensions to evaluate program success in real-world settings.
- Medical Research Council (MRC) Framework for Complex Interventions: The MRC framework provides guidance for developing and evaluating complex interventions through stages of development, feasibility and piloting, evaluation, and implementation.
- SELFIE Model (Sustainable intEgrated chronic care modeLs for multi-morbidity: delivering, FInancing, performancE): This framework, aligned with WHO health system components, focuses on the sustainability of integrated care models, considering leadership, service delivery, resources, and information systems.
- Define, Measure, Analyze, Improve, Control (DMAIC) Quality Improvement Methodology: A structured approach to quality improvement, DMAIC focuses on process optimization and data-driven decision-making.
The increasing adoption of these frameworks in recent studies underscores a growing recognition of the importance of systematic implementation strategies in palliative care. Utilizing these frameworks ensures a comprehensive approach, moving beyond simply demonstrating the benefits of palliative care to actively embedding it within routine oncology practice.
Key Enablers for Successful Palliative Care Program Implementation
Building a thriving hospital-based palliative care program requires cultivating an environment that supports its integration and sustainability. Several key enablers emerged from the reviewed studies as crucial for program success:
Dedicated and Competent Staff
- Specialized Palliative Care Team: The availability of a dedicated palliative care team, including physicians, nurses, and other allied health professionals, is paramount. This team provides specialized expertise, ensuring timely response to consultations and effective management of complex patient needs. The “Clinical Provider of the Day” model, for instance, demonstrates how dedicated staffing can significantly increase capacity for urgent palliative care consults.
- Clearly Defined Roles: Well-defined roles and responsibilities for both palliative care specialists and oncology staff are essential. Oncologists often perceive palliative care as a collaborative partnership, with palliative care teams taking primary responsibility for symptom management and psychosocial support, while oncologists focus on cancer-directed treatments. Clarity in roles fosters effective collaboration and reduces role ambiguity.
- Building Healthcare Provider Confidence: Integrating palliative care improves oncologist confidence in delivering palliative care and initiating advance care planning discussions. Educational initiatives and training programs play a crucial role in enhancing provider skills and comfort in addressing palliative care needs.
Patient-Centered Approach and Education
- Positive Patient Perceptions: When patients and caregivers understand the benefits of palliative care, they are more likely to engage positively with the program. Satisfied patients and caregivers often highlight improved symptom management, holistic support, and assistance with decision-making as key benefits.
- Addressing Stigma: The term “palliative care” can carry stigma, often associated with end-of-life care only. Programs must proactively address this misconception through education and clear communication, emphasizing that palliative care is about improving quality of life at any stage of serious illness, not just at the very end of life.
System Integration and Support
- Workflow Integration: Seamless integration of palliative care into existing hospital workflows and electronic health record systems is critical. Embedding palliative care within established routines minimizes disruption and maximizes efficiency.
- Administrative Support: Strong administrative support, including dedicated time, funding, and human resources, is indispensable. Visible support from senior management and tumor stream leaders signals organizational commitment and provides the necessary resources for program implementation and sustainability.
- Organizational Culture and Education: Fostering a supportive organizational culture that values interdisciplinary collaboration and continuous learning is essential. Multidisciplinary teams, palliative care training for all relevant staff, and recognition of clinical champions all contribute to a positive and supportive environment for palliative care integration.
- Effective Communication: Open and timely communication between palliative care teams, oncology staff, patients, and caregivers is vital. Establishing clear communication channels and protocols ensures coordinated care and timely access to palliative care services. “Warm Handoff” programs, where oncologists directly introduce patients to palliative care nurses, are effective strategies for enhancing communication and referral processes.
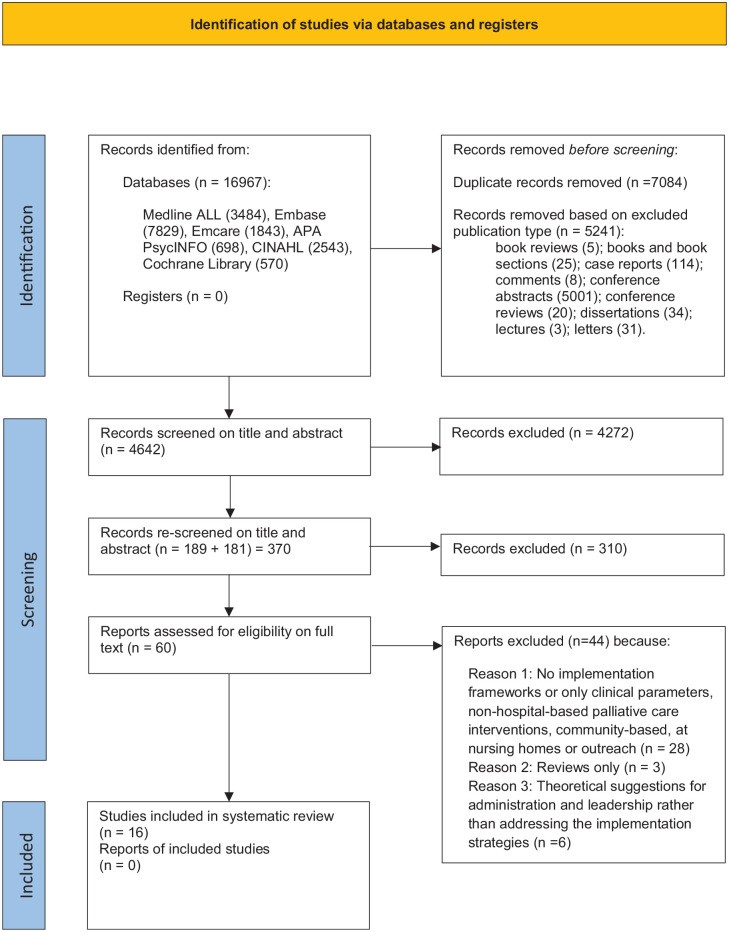 Figure 1.
Figure 1.
Overcoming Barriers to Palliative Care Program Development
Despite the recognized benefits and identified enablers, implementing hospital-based palliative care programs often faces significant challenges. Understanding these barriers is crucial for proactive mitigation and strategic program design:
Staff-Related Barriers
- Lack of Dedicated Staff: Insufficient staffing levels, particularly specialized palliative care professionals, can limit program reach and effectiveness.
- Unclear Roles and Responsibilities: Ambiguity regarding roles between oncology and palliative care teams can lead to inefficiencies, duplicated efforts, or gaps in care.
- Inadequate Training and Education: Lack of robust palliative care training for both specialist and non-specialist staff can hinder program implementation and quality of care. This includes training in communication skills for sensitive conversations.
- Rapid Staff Turnover: High staff turnover in hospital settings disrupts program continuity, necessitates ongoing training efforts, and can negatively impact data collection and established relationships.
Patient-Related Barriers
- Stigma Associated with Palliative Care: Negative perceptions and associations of palliative care with imminent death can deter patients and families from seeking or accepting early palliative care services.
- Patient Understanding and Engagement: Ensuring patients and families fully understand the goals and benefits of palliative care is crucial for engagement and program acceptance. Complexity of hematologic malignancies can sometimes make patient interest in palliative care research lower, impacting feedback collection, as noted in some studies.
System-Related Barriers
- Workflow Disruption: Integrating new palliative care processes can disrupt existing workflows and clinical routines if not carefully planned and implemented.
- Administrative Hurdles: Securing adequate time, funding, and physical space for palliative care programs can be challenging within resource-constrained hospital environments.
- Lack of Policy Support and Financial Schemes: Insufficient health policy regulations and dedicated financial mechanisms to support palliative care services can hinder program sustainability.
- Communication Gaps: Breakdowns in communication between healthcare teams, patients, and caregivers can impede effective palliative care integration.
- Institutional Review Board (IRB) Processes: Complex or inconsistent IRB processes for palliative care research and quality improvement initiatives can create barriers to program evaluation and refinement.
Implementation Guideline Barriers
- Maintaining Fidelity and Consistency: Ensuring consistent implementation of palliative care interventions across diverse patient populations and hospital sites can be challenging.
- Lack of Benchmark Criteria: The absence of clear, standardized benchmarks for assessing palliative care program implementation and impact makes it difficult to measure success and drive continuous improvement.
Practical Strategies: Applying the RE-AIM Framework for Palliative Care Program Building
The RE-AIM framework provides a practical structure for organizing strategies to address both enablers and barriers in palliative care program implementation. By considering each dimension of RE-AIM, program developers can create a comprehensive and impactful plan.
Reach: Who will be impacted, and how will you ensure broad access?
- Enablers:
- Develop an integrated palliative care model collaboratively with providers, administrators, patients, and family advisors to ensure relevance and acceptance.
- Prioritize maintaining strong physician-patient relationships to facilitate early palliative care integration and address end-of-life care needs sensitively.
- Promote palliative care conversations proactively between doctors and patients.
- Barriers & Strategies:
- Address lack of awareness through public and professional education campaigns about the benefits of early palliative care.
- Involve multidisciplinary teams in outreach and education efforts to broaden program reach.
Effectiveness: Is the program achieving its goals?
- Enablers:
- Ensure dedicated program staff, including palliative care specialists, are available.
- Invest in comprehensive, interactive training programs for healthcare professionals, led by palliative care experts.
- Implement an integrated palliative care model that facilitates timely, efficient, and coordinated interdisciplinary care.
- Prioritize co-design of interventions, incorporating feedback from patients, caregivers, and providers to enhance program effectiveness.
- Embed the palliative care program within existing workflows and electronic health record systems for seamless integration.
- Adopt a multidisciplinary approach with appropriate timing and resources to address the needs of medically and socially complex patients.
- Barriers & Strategies:
- Address communication barriers by providing training in end-of-life communication for physicians and staff.
- Challenge physician perceptions that equate palliative care solely with end-of-life care through education and data showcasing the broader benefits.
- Mitigate administrative barriers by securing dedicated time and resources for program implementation and ongoing operation.
- Provide robust training for the palliative care team and clearly define roles to ensure effective program delivery.
Adoption: Will the program be adopted by the target settings and staff?
- Enablers:
- Establish Community Advisory Groups to oversee program monitoring and evaluation, fostering community ownership.
- Utilize co-design principles, engaging key clinical partners in program development to ensure relevance and buy-in.
- Gather real-time qualitative feedback from oncologists and adapt the program iteratively to enhance uptake.
- Embed palliative care within the very systems of cancer care, making it a routine part of oncology services.
- Assess organizational readiness for change through surveys and workflow analysis prior to service implementation.
- Develop comprehensive materials and resources to facilitate program delivery and adoption.
- Leverage frameworks like SELFIE, which emphasize sustainability through post-discharge follow-up, new role creation, and continuous feedback loops.
- Barriers & Strategies:
- Address physician perceptions that limit palliative care to end-of-life by showcasing evidence of broader benefits and early integration models.
- Minimize workflow disruption by carefully integrating the program into existing clinical practice and routines.
Implementation: Is the program delivered as intended?
- Enablers:
- Integrate palliative care seamlessly into existing workflows, electronic systems, and dedicated staffing networks.
- Commit dedicated time, funding, and human resources to program implementation.
- Utilize training interventions to facilitate adjustments to clinical care pathways within tumor boards and multidisciplinary teams.
- Establish clear roles and responsibilities for all involved clinicians (oncologists and palliative care physicians).
- Utilize quality indicators to monitor and guide program implementation.
- Integrate the palliative care team into the hospital information system (HIS) for efficient communication and data sharing.
- Document goals of care documentation rates post-implementation to track progress and impact.
- Barriers & Strategies:
- Develop sustained implementation strategies and guidelines, drawing upon frameworks and best practices.
- Raise awareness of formal implementation policies and procedures.
- Address practical barriers like access to guidelines, time constraints, and resistance to changing established routines.
- Advocate for a standardized IRB approach to facilitate efficient program evaluation.
- Mitigate the impact of rapid staff turnover through robust onboarding and training programs.
- Develop strategies to maintain fidelity and consistency of the intervention across diverse settings and patient populations, such as standardized protocols and ongoing training.
Maintenance: Can the program be sustained over time?
- Enablers:
- Balance palliative care referral volume with available staff resources to prevent burnout and maintain service quality.
- Recognize and celebrate clinical champions who advocate for and support the palliative care program.
- Barriers & Strategies:
- Advocate for relevant health policy regulations and financial schemes to ensure long-term funding and sustainability of palliative care services.
- Establish clear benchmark criteria to assess palliative care implementation and impact, enabling ongoing monitoring and quality improvement.
Conclusion: Embracing Implementation Science for Sustainable Palliative Care Programs
This guide underscores the critical need for a systematic approach to building hospital-based palliative care programs. While the evidence base for early palliative care is strong, translating this evidence into widespread practice requires a concerted effort grounded in implementation science principles.
By understanding and addressing the key enablers and barriers outlined in this guide, and by strategically applying implementation frameworks like RE-AIM, healthcare organizations can develop effective, sustainable, and patient-centered palliative care programs. Focusing on co-design, staff education, dedicated resources, and clear communication is paramount. Embracing implementation science is not merely an academic exercise but a practical imperative for ensuring that all patients with advanced cancer benefit from timely and comprehensive palliative care, enhancing their quality of life and overall care experience. The future of palliative care integration lies in the deliberate and informed application of these frameworks to guide service development and ensure lasting impact.
References
[References] (Please use the original article’s references here, ensuring they are correctly formatted in markdown)