Chronic Care Management (CCM) programs have emerged as a vital strategy in modern healthcare, particularly for the growing population of individuals managing multiple chronic conditions. While the primary goal of CCM is to enhance patient care and health outcomes, a significant and increasingly recognized benefit is their ability to generate substantial cost savings. This article delves into how CCM programs effectively save money, drawing on evidence-based research and practical applications.
Understanding Chronic Care Management and Its Economic Impact
The Centers for Medicare & Medicaid Services (CMS) introduced Chronic Care Management as a distinct Medicare benefit in 2015, acknowledging the critical need for ongoing support for patients with two or more chronic conditions expected to last at least a year. These individuals, often representing a significant portion of the Medicare fee-for-service population, frequently encounter healthcare needs between traditional office visits. CCM programs bridge this gap by providing structured, non-face-to-face care management services.
A landmark study commissioned by CMS itself investigated the initial 18 months of the CCM program and revealed compelling results regarding its economic impact. The research demonstrated that CCM not only improved care planning and healthcare utilization but also led to significant cost reductions. Specifically, after excluding patients with minimal CCM engagement, the study found that CCM participation resulted in Medicare savings of $95 per patient per month compared to a control group not receiving CCM. Accounting for the cost of CCM services, the estimated net savings for CMS surpassed $38 million. This striking finding underscores the inherent cost-effectiveness of CCM programs, even with varied implementation approaches across healthcare practices.
Key Mechanisms Through Which CCM Programs Drive Cost Savings
The economic benefits of CCM programs are multifaceted, stemming from their proactive and comprehensive approach to patient care. Several key mechanisms contribute to these cost savings:
1. Reduction in Hospitalizations and Emergency Department Visits
One of the most significant areas of cost savings associated with CCM programs is the reduction in avoidable hospitalizations and emergency department (ED) visits. Individuals with chronic conditions are at higher risk of acute exacerbations requiring urgent or emergent care. CCM programs proactively address this risk through:
- Risk Assessment and Early Intervention: CCM programs utilize evidence-based risk assessments to identify patients at high risk of hospitalization. By proactively monitoring and addressing these risks, care managers can intervene early to prevent health deteriorations that might otherwise lead to hospital admissions. For instance, in a study of 26,500 patients receiving CCM support, a technology-enabled platform was used to flag patients at high risk for hospitalization. While counterintuitive at first glance, patients identified as high-risk in this system actually experienced lower hospitalization rates, suggesting that proactive risk identification and communication facilitated timely interventions.
- Enhanced Medication Management: Polypharmacy, common among individuals with multiple chronic conditions, significantly increases the risk of adverse drug events and subsequent hospitalizations. CCM programs incorporate thorough medication reconciliation, adherence reviews, and management of potential drug interactions. By optimizing medication regimens and ensuring proper adherence, CCM can prevent medication-related complications that often necessitate costly hospital care.
- Improved Care Coordination and Transitions: Fragmented care is a major contributor to adverse events and avoidable hospital readmissions. CCM programs emphasize seamless care coordination across different healthcare settings and providers. This includes managing care transitions after hospital discharges or ED visits and ensuring timely follow-up care, which is crucial in preventing readmissions and associated costs.
2. Proactive Management of Chronic Conditions
CCM programs are designed to provide continuous, proactive management of chronic conditions, rather than reactive care focused solely on episodic illness. This proactive approach yields economic benefits by:
- Preventing Disease Progression: Regular monitoring, patient education, and support for self-management empower patients to actively participate in their care and adhere to treatment plans. This can slow disease progression, reduce the incidence of complications, and decrease the need for intensive and expensive treatments in the long term.
- Promoting Preventive Care: CCM programs ensure that patients receive all recommended preventive services, such as vaccinations and screenings. Preventive care is widely recognized as a cost-effective healthcare strategy, as it can detect diseases early when they are more treatable and less costly to manage.
- Addressing Unmet Needs: CCM programs incorporate systematic assessments of patients’ medical, functional, and psychosocial needs. By identifying and addressing unmet needs, such as social determinants of health or mental health concerns, CCM can prevent these issues from escalating into more complex and costly health problems.
3. Efficient Use of Healthcare Resources
CCM programs promote a more efficient allocation of healthcare resources by:
- Substituting Non-Face-to-Face Care for Office Visits: CCM services are primarily delivered through non-face-to-face modalities, such as telephone, secure messaging, and virtual care platforms. This reduces the demand for in-person office visits, freeing up physician time for patients requiring direct medical attention. Non-face-to-face care is generally less expensive than office visits, contributing to overall cost savings.
- Utilizing a Team-Based Care Approach: CCM programs often employ a team-based care model, involving nurses, medical assistants, and other healthcare professionals working under the supervision of a physician. This allows for task delegation and efficient use of clinical staff, optimizing the cost-effectiveness of care delivery.
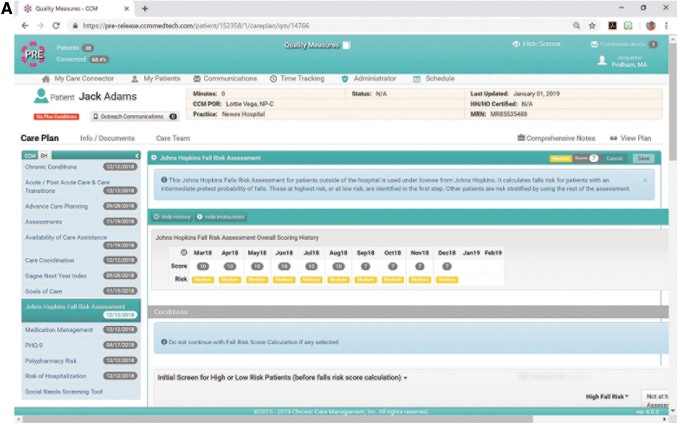
- Leveraging Technology for Scalability and Efficiency: Technology platforms designed to support CCM workflows enhance efficiency and scalability. These platforms can automate data collection, risk stratification, care planning, and communication, reducing administrative burden and improving care coordination. The ability to manage a larger patient population efficiently through technology contributes to the economic viability of CCM programs.
Evidence of Cost Savings: Data and Research
Beyond the initial CMS-commissioned study, further research reinforces the cost-saving potential of CCM programs. Studies have demonstrated:
- Reduced Medicare Expenditures: Analyses of Medicare claims data have shown that beneficiaries enrolled in CCM programs experience lower overall Medicare expenditures compared to similar beneficiaries not enrolled in CCM. These savings are often attributed to reductions in hospitalizations, ED visits, and skilled nursing facility stays.
- Return on Investment (ROI): Several healthcare organizations implementing CCM programs have reported positive ROIs, indicating that the savings generated by CCM outweigh the program costs. The ROI is influenced by factors such as program design, patient population, and healthcare setting, but the overall trend points towards a favorable economic return.
- Value-Based Care Alignment: CCM programs are well-aligned with the principles of value-based care, which emphasizes quality and cost-effectiveness. By improving health outcomes and reducing costs, CCM programs contribute to the shift from fee-for-service to value-based payment models.
Implementing Cost-Effective CCM Programs
To maximize the cost savings of CCM programs, healthcare organizations should consider the following:
- Target High-Risk Populations: Focus CCM program enrollment on individuals with multiple chronic conditions who are at highest risk of hospitalization or other adverse events. This targeted approach ensures that CCM resources are directed to those who are most likely to benefit from proactive care management and generate cost savings.
- Integrate Evidence-Based Protocols and Tools: Utilize evidence-based risk assessments, care plans, and workflow modules to guide CCM program delivery. Standardized, evidence-based approaches enhance program effectiveness and ensure consistent, high-quality care.
- Leverage Technology Strategically: Implement technology platforms that streamline CCM workflows, automate tasks, and facilitate data-driven care management. Technology is crucial for scalability, efficiency, and maximizing the economic benefits of CCM programs.
- Track and Measure Outcomes: Establish robust data collection and analysis systems to track key outcomes, including hospitalizations, ED visits, healthcare costs, and patient satisfaction. Regular monitoring and evaluation are essential for demonstrating the value of CCM programs and identifying areas for improvement.
Conclusion: CCM Programs as a Financially Sound Healthcare Investment
Chronic Care Management programs are not only beneficial for improving the health and well-being of individuals with chronic conditions but also represent a sound financial investment for healthcare systems. By proactively managing chronic illnesses, reducing avoidable hospitalizations, and promoting efficient resource utilization, CCM programs generate significant cost savings. As healthcare continues to evolve towards value-based care models, CCM programs are poised to play an increasingly important role in delivering high-quality, cost-effective care for the growing population managing chronic diseases. The evidence clearly demonstrates that investing in well-designed and implemented CCM programs is a strategic approach to achieving both improved patient outcomes and substantial financial returns.