Millions of individuals in the United States grapple with serious illnesses that diminish their quality of life, marked by distressing symptoms and significant caregiver burden. In response to these critical needs, palliative care has emerged as a vital, team-based medical specialty. Palliative care focuses on enhancing the quality of life for both patients and their families facing serious illness. It has proven its effectiveness in improving care quality while potentially reducing costs compared to standard hospital care. Understanding How Many Hospitals Have Palliative Care Programs is crucial for ensuring widespread access to this essential service.
Building upon previous research indicating that 67% of U.S. hospitals with 50 or more beds had palliative care programs by 2013, this updated analysis investigates the prevalence of these programs as of 2017. It further explores the hospital and market factors associated with their presence. A clear understanding of the variations in palliative care program availability across U.S. hospitals is paramount to improving care for those with serious illnesses and their families. This study aims to shed light on the current landscape of palliative care in hospitals and identify areas for improvement in accessibility and equity.
To conduct this comprehensive analysis, data was gathered from the American Hospital Association (AHA) Annual Survey Database™ for 2017, supplemented with 2016 data for non-responding hospitals. This database provides self-reported information from hospitals regarding their available facilities and services, including inpatient palliative care. To enrich the dataset, the AHA data was linked with the United States Census Bureau’s 2017 American Community Survey at the county level. Furthermore, the Dartmouth Atlas of Health Care’s 2016 Spending and 2011 Hospital and Physician Capacity datasets were incorporated at the health services area level to capture health care market and geographic characteristics.
The study focused on a sample of hospitals with 50 or more beds, excluding federal hospitals, and including general medical and surgical, children’s, cancer, heart, and obstetrics and gynecology hospitals within the 50 states and the District of Columbia. To ensure data accuracy, the palliative care program status reported in the AHA database was verified against multiple sources. These sources included the National Palliative Care Registry™, state-level palliative care directories, health system palliative care contacts, and extensive web-based searches. Multivariable logistic regression models and average marginal effects were employed to analyze the relationships between the presence of inpatient palliative care programs and various factors. These factors encompassed hospital characteristics, community-level socioeconomic demographics, health care markets, and geographic characteristics.
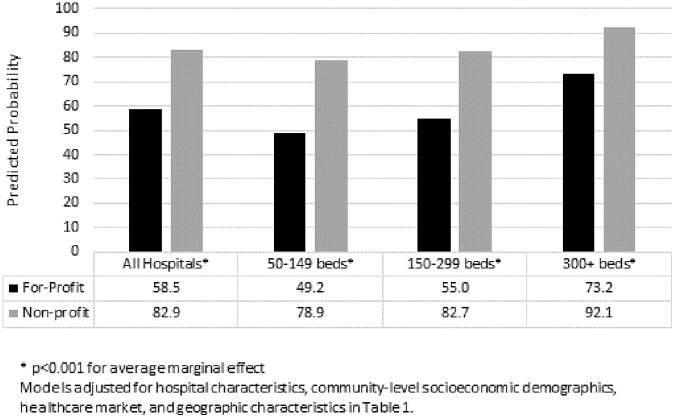 Predicted probability of having a palliative care program by hospital size and ownership. This graph shows that larger and non-profit hospitals are more likely to offer palliative care programs, highlighting disparities in access based on hospital characteristics.
Predicted probability of having a palliative care program by hospital size and ownership. This graph shows that larger and non-profit hospitals are more likely to offer palliative care programs, highlighting disparities in access based on hospital characteristics.
The study revealed that out of 2409 U.S. hospitals analyzed, 1723, or 71.5%, reported having palliative care programs. Consistent with previous findings, the availability of hospital palliative care demonstrated significant variations based on hospital characteristics and geographic factors. Hospital ownership emerged as a critical factor, with nonprofit hospitals being significantly more likely to offer palliative care compared to for-profit hospitals. Specifically, nonprofit hospitals were 24.5 percentage points more likely to have palliative care programs. Geographic location also played a substantial role. Hospitals in metropolitan areas were 15.4 percentage points more likely to have palliative care programs compared to those in rural areas. These disparities highlight the influence of hospital type and location on the accessibility of palliative care services.
The research underscores that while a substantial number of hospitals, approximately 72% of those with 50 or more beds, offer palliative care programs, significant disparities persist based on hospital type. Notably, for-profit hospitals lag significantly behind nonprofit and public hospitals in providing palliative care. This ownership-based difference is particularly pronounced in smaller hospitals. Despite the slower adoption rate compared to nonprofit and public institutions, there has been a positive trend with for-profit hospitals showing a 12 percentage point increase in palliative care program prevalence since 2013. Regionally, the west south central region continues to have one of the lowest palliative care prevalence rates, but it has also demonstrated the most significant regional growth, with an 8 percentage point increase since 2013.
Several factors may contribute to the observed variations in palliative care program availability. These include a potential shortage of palliative care professionals, inadequate funding and incentives for program development, a lack of systematic accountability for ensuring palliative care access, and ongoing gaps in awareness and understanding of palliative care’s benefits. It is important to note that this study focused on the presence of palliative care programs and did not evaluate the quality, scope, or size of these services, which are known to vary considerably. Despite these limitations, the findings highlight the urgent need for targeted strategies to address the existing gaps in hospital palliative care availability. Ensuring equitable and reliable access to quality palliative care across the nation is essential to meet the needs of millions of Americans living with serious illnesses and their families.

