Nursing care plans serve as a strategic framework to streamline the nursing process and enhance communication within healthcare teams. They are essential tools for outlining patient needs and ensuring holistic care. This guide delves into the fundamentals of nursing care plans and provides a step-by-step approach to creating effective programs, incorporating best practices and offering a downloadable example for practical application.
Understanding Nursing Care Plans
A nursing care plan is a documented strategy that details how to identify a patient’s specific needs and deliver holistic care. It typically follows a structured, five-step framework, promoting collaboration among nurses, patients, and other healthcare providers. A well-structured care plan ensures a coordinated and patient-centered approach to healthcare delivery.
The Core Objectives of Nursing Care Plans
The primary purpose of a nursing care plan is to comprehensively document a patient’s needs, preferences, and the planned nursing interventions or actions designed to address those needs. As a vital component of the patient’s health record, the care plan establishes and maintains continuity of care across the healthcare spectrum. Several key reasons underscore the importance of developing robust care plans:
Patient-Centered Approach
Care plans are instrumental in helping nurses and the broader care team organize and manage patient care in a structured, timeline-oriented manner. They serve as a framework for critical and holistic thinking, ensuring that patient care encompasses physical, psychological, social, and spiritual dimensions. Furthermore, Nursing Care Plan Programs facilitate the efficient assignment of patients to nurses with the most appropriate skills and experience. For patients, clearly defined goals outlined in a care plan can significantly enhance their engagement and active participation in their treatment and recovery journey.
Fostering Nursing Team Collaboration
The development and implementation of a nursing care plan encourage seamless collaboration among nurses, physicians, assistants, and other healthcare providers. By providing a centralized repository of patient information, care plans enable team members to share insights, exchange opinions, and collectively contribute to delivering optimal patient care.
Documentation and Regulatory Compliance
A meticulously crafted nursing care plan serves as a tool for nurses to evaluate the effectiveness of the care provided and to maintain a clear record of care delivery. This documentation is crucial for optimizing care efficiency, ensuring accountability, and meeting healthcare provider documentation requirements.
Key Components of Nursing Care Plan Programs: A Five-Step Framework
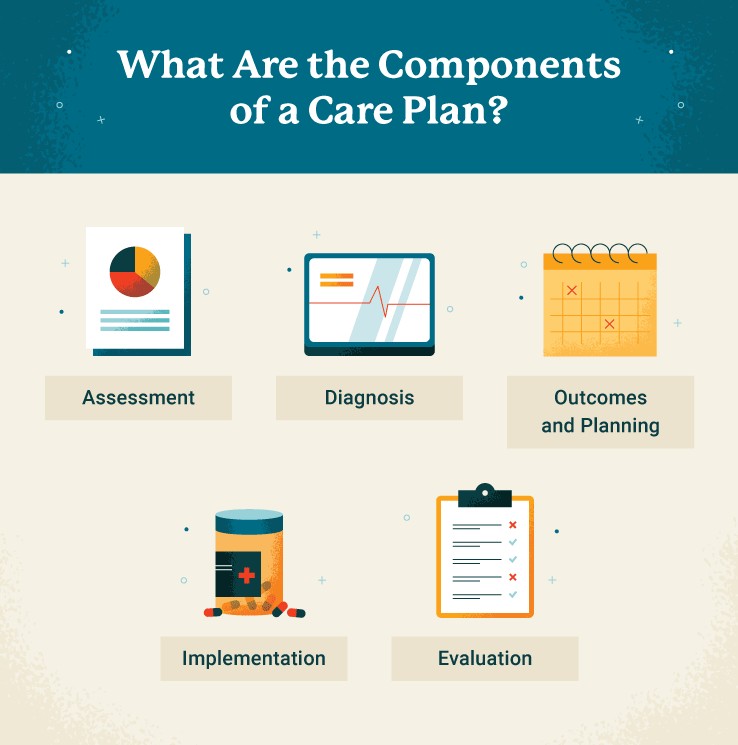
Nursing care plan programs are typically organized around a five-step framework, providing a systematic approach to patient care. These steps include assessment, diagnosis, outcomes and planning, implementation, and evaluation.
Step 1: Comprehensive Patient Assessment
The initial step in developing a nursing care plan program involves a thorough patient assessment, requiring critical thinking and meticulous data collection. While specific formats may vary across healthcare organizations, the assessment phase generally involves gathering both subjective and objective data. Subjective data includes patient statements and reported symptoms, while objective data encompasses measurable information such as vital signs, physical measurements, and intake/output records. Sources of subjective data can include patients themselves, family members, caretakers, and close friends.
Nurses play a vital role in collecting data on vital signs, physical complaints, observable conditions, medical history, and neurological function. The integration of digital health records can streamline the assessment process by automatically populating relevant patient information from previous encounters.
Step 2: Formulating a Nursing Diagnosis
The second step involves formulating a nursing diagnosis based on the data collected during the assessment phase. According to NANDA International Inc. (NANDA-I), a nursing diagnosis is defined as “a clinical judgment about the human response to health conditions/life processes, or a vulnerability for that response, by an individual, family, group or community.”
The nursing diagnosis serves as the foundation for selecting appropriate nursing actions and interventions to achieve specific patient outcomes. This diagnostic process is often grounded in Maslow’s Hierarchy of Needs, a psychological theory that prioritizes human needs to guide effective treatment strategies. In the context of nursing care plan programs, physiological needs, such as food, water, and respiration, take precedence over higher-level needs like love, belonging, esteem, and self-actualization, ensuring that basic survival needs are addressed first in nursing interventions.
Based on the established nursing diagnosis, the subsequent steps (Step 3 and 4) involve setting patient-centered goals and planning nursing implementations to effectively resolve the identified patient problems.
Step 3: Defining Outcomes and Planning Strategies
Following the diagnosis, the planning stage in nursing care plan programs focuses on defining desired patient outcomes and developing strategic interventions. This stage involves establishing SMART goals, which are Specific, Measurable, Achievable, Realistic, and Time-bound, based on evidence-based practice (EBP) guidelines. Careful consideration is given to the patient’s overall condition, diagnosis, and other pertinent information to ensure that the goals set are both desirable and realistically attainable within short-term and long-term timeframes.
Step 4: Implementing Nursing Interventions
Once patient-centered goals are clearly defined, the implementation phase involves putting the planned actions into practice to support patients in achieving these goals. This stage of the nursing care plan program focuses on performing the specific nursing interventions outlined in the care plan. Nurses typically follow physician orders for interventions or develop their own interventions based on established evidence-based practice guidelines and protocols.
Nursing interventions are broadly categorized into seven domains: family, behavioral, physiological, complex physiological, community, safety, and health system interventions. Routine interventions that are often implemented during each nursing shift include pain assessment, repositioning, active listening, cluster care to minimize disruptions, fall prevention measures, and promoting adequate fluid intake.
Step 5: Ongoing Evaluation and Adjustment
The final step in the nursing care plan program is the evaluation phase. During this stage, healthcare professionals, including nurses and physicians, assess whether the desired patient outcomes have been achieved. The findings of this evaluation inform necessary adjustments to the nursing care plan to optimize its effectiveness. This iterative process ensures that the care plan remains dynamic and responsive to the patient’s evolving needs.
Fundamental Principles of Effective Care Plan Programs
Nurse.org highlights the core questions that every effective care plan should answer: what, why, and how. A robust nursing care plan program should clearly define:
- The What: What health issues is the patient currently experiencing? What potential health risks does the patient face?
- The Why: What are the underlying causes of the patient’s current health issues? What factors contribute to the patient’s potential health risks?
- The How: What nursing interventions and strategies can be implemented to improve the patient’s condition and mitigate risks?
Successful nursing care plan programs are built upon fundamental principles including critical thinking, patient-centered techniques, goal-oriented strategies, evidence-based practice (EBP) recommendations, and informed nursing intuition.
SMART Goal Setting in Care Plans
Goal-oriented strategies are central to effective nursing care plan programs. Utilizing a SMART goals framework is crucial for ensuring that patient goals are well-defined and actionable:
- Specific: Patient goals must be clearly defined, leaving no room for ambiguity.
- Measurable: Specific metrics should be established to track and measure patient progress toward goal achievement.
- Achievable: Goals set for patients should be realistically achievable, considering their overall condition and circumstances.
- Realistic: Goals must be relevant to the patient’s care plan and attainable within the context of their health status and resources.
- Time-bound: Each patient goal should have a clearly defined start date and an anticipated end date, allowing for progress monitoring and adjustments as needed.
The Importance of Effective Communication
A well-developed care plan is only effective if it is effectively communicated to all relevant stakeholders. Nursing care plan programs are not static documents but rather dynamic tools intended to guide the nursing process, promote teamwork, and ultimately enhance patient care. Strong writing and communication skills are essential for nurses to ensure accuracy and clarity in care plan documentation. To facilitate effective communication, consider these best practices when developing and implementing care plans:
- Document information promptly to ensure accuracy and prevent loss of detail.
- Write clearly and concisely, using terminology that is readily understood by all members of the healthcare team.
- Include precise dates and times for all relevant entries and interventions.
While communication skills are developed through undergraduate and graduate nursing programs, practical experience and ongoing professional development further refine these crucial competencies.
Accessibility and Shareability of Care Plans
Nursing care plans need to be easily accessible and readily shareable with all relevant stakeholders, including patients, physicians, other nurses, insurance providers, and other members of the care team. Documentation formats may vary based on specific hospital policies and regulatory requirements. Typically, nursing care plans are created and maintained in electronic format, integrated within the electronic health record (EHR) system to ensure seamless access for authorized personnel.
Maintaining Up-to-Date Care Plans
Regularly updating nursing care plans with the most current patient information is essential for their ongoing effectiveness. Frequent check-ins with patients and meticulous recording of progress toward established goals are critical steps in preparing for the evaluation stage of the care plan program. Consistent updates ensure that the care plan remains relevant, responsive, and reflective of the patient’s current health status and evolving needs.
Nursing Care Plan Examples: Student vs. Professional Practice
It is important to note that nursing care plan examples developed by students often differ significantly from those created by experienced registered nurses in clinical settings. Student care plans tend to be more detailed, comprehensive, and exhaustive, reflecting their learning process. In contrast, practicing nurses often rely on their extensive experience and may mentally note certain steps or assume basic concepts, resulting in more concise care plans.
For example, in the interventions section, a student might write: “Vital signs recorded every four hours: blood pressure, heart rate, three- or five-lead electrocardiograms, functional oxygen saturation, respiratory rate, and skin temperature,” whereas a registered nurse might simply document “Q4 vital signs.”
This difference stems from the learning objectives of each group. For students and recent graduates, including detailed information in care plans reinforces their training and solidifies their understanding of the nursing process. While creating detailed nursing care plan examples in an academic setting can be time-consuming, mastering this skill during nursing school is crucial for building competency and confidence in professional practice. Information that requires frequent look-up during training gradually becomes second nature with experience.
Here is a simplified care plan example that a student might develop:
- Assessment: “Heart rate 100 bpm, dyspnea, restlessness, guarding behavior observed.”
- Diagnosis: “Impaired gas exchange related to collection of mucus in the airway.”
- Outcomes and Planning: “Patient will maintain optimal gas exchange throughout care.”
- Implementations: “Assess respiratory status every 2 hours; encourage deep breathing and position changes every hour.”
- Rationale: “Regular respiration assessment will indicate the level of lung involvement and effectiveness of interventions; deep breathing and position changes promote ventilation and chest expansion, facilitating gas exchange.”
- Evaluation: “Patient maintained good gas exchange and normal respiratory rate throughout the shift.”
Student nursing care plans often include a “rationale” column, where students articulate the scientific reasoning behind their chosen interventions, further solidifying their understanding of evidence-based practice. To support care plan writing practice, a printable nursing care plan example is readily available, providing a template for practicing each step outlined in this guide.
Conclusion: Optimizing Nursing Care Through Effective Programs
For nursing care plans to be truly effective, they must prioritize clear communication, incorporate goal-oriented tasks, ensure accessibility and shareability, and be grounded in evidence-based practice.
When these essential qualities are combined with the nurse’s intuition, critical thinking abilities, and a patient-centered focus, nursing care plan programs become invaluable resources for nurses to document, access, and utilize critical patient information. A well-designed care plan serves as a roadmap for delivering effective nursing care and a collaborative tool that enhances the entire healthcare process.
While all nursing programs provide foundational training in care plan development, the depth of skill in communication, goal setting, and critical thinking is shaped by the specific program curriculum and learning experiences. Nursing care plan programs play a vital role in fostering professional development, instilling core values such as accountability, respect, and integrity. These professional attributes ultimately contribute to improved patient care, enhanced team communication, and a more positive and effective work environment within healthcare settings.
Choosing the right nursing program is crucial for developing the essential skills in communication, critical thinking, and professionalism necessary for success in the dynamic field of nursing.
The University of St. Augustine for Health Sciences (USAHS) offers a Master of Science in Nursing (MSN), a Doctor of Nursing Practice (DNP) and Post-Graduate Nursing Certificates designed for working nurses. Our degrees are offered online, with optional on-campus immersions.* Role specialties include Family Nurse Practitioner (FNP), Psychiatric Mental Health Nurse Practitioner (PMHNP)** and Nurse Executive. The MSN and DNP have options to accelerate your time to degree completion. Earn your advanced nursing degree while keeping your work and life in balance.
*The FNP role specialty includes one required hands-on clinical intensive as part of the curriculum.
**The Psychiatric Mental Health Nurse Practitioner role specialty is not available for the DNP program.