Navigating the complexities of long-term care in today’s environment, marked by persistent nurse shortages and increased demands on healthcare professionals, can often lead to the oversight of crucial programs like restorative nursing. However, the strategic implementation of restorative programs within long-term care facilities is not merely beneficial for enhancing the quality of life for residents; it also represents a significant avenue for financial reimbursement. The pressing question then becomes: how can long-term care facilities effectively integrate restorative programming amidst the current challenges they face? This article aims to provide comprehensive insights and answers.
Defining Restorative Nursing Programs in Long Term Care
The definitive guide for restorative nursing programs, often referred to as RNPs, is the RAI (Resident Assessment Instrument) Manual. According to this manual, restorative nursing programs are defined as:
“nursing interventions that promote the resident’s ability to adapt and adjust to living as independently and safely as possible. This concept actively focuses on achieving and maintaining optimal physical, mental, and psychosocial functioning.” – MDS 3.0, RAI manual
In practical terms, a Restorative Nursing Program (RNP) is a structured, formalized, and carefully planned care approach designed to either recover a lost capability or sustain a function at risk of decline for a specific resident in long term care. According to restorative care expert, Nicole Watson, “This type of programming is a vital component to individualizing one’s care. They’re more than just normal nursing or custodial care, it’s person-centered versus traditional care.” This distinction underscores the proactive and personalized nature of RNPs in enhancing resident independence and well-being within long term care settings.
The Necessity of Restorative Nursing Programs in Long Term Care Facilities
While regulatory mandates may not explicitly require the implementation of Restorative Nursing Programs (RNPs) in long term care facilities, the substantial advantages they offer to both residents and the facilities themselves make them an undeniably wise choice. Some might perceive RNPs as supplementary to essential care, thus overlooking their potential. Concerns about insufficient staffing to manage even basic care, let alone additional programs, are frequently voiced. However, it’s crucial to recognize that RNPs can be seamlessly woven into the daily care routines already performed by nursing teams. Often, it’s a matter of properly documenting existing practices that foster resident independence, thereby acknowledging and receiving due reimbursement for these efforts.
The true necessity of RNPs hinges on perspective. As Nicole Watson aptly puts it, “If you can get your staff to think of restorative programs as the foundation of your individualized resident care, it actually becomes part of your culture and your mission to help people live the best quality that they can at this stage in their lives, which is truly why most of us are in this industry; because we want to enhance the lives of our elders. So, making [RNPs] part of your culture and ingraining it in your foundation and in your nursing practice makes it easier.”
Therefore, restorative programming should not be viewed as an optional extra in long term care, but rather as an integral and essential element for delivering effective and successful care. It is fundamental to a resident-centered approach in long term care.
The Core Importance of RNPs in Long Term Care
To truly appreciate the value of Restorative Nursing Programs (RNPs) in long term care, it’s beneficial to consider the resident’s perspective. Admission to a Skilled Nursing Facility (SNF) or similar sub-acute care community often entails significant loss for residents, both tangible and emotional. They may transition from a familiar, spacious home filled with personal belongings to a nursing environment with restricted space and fewer personal freedoms. They might have experienced the loss of independence in driving, the constant companionship of a partner, or their established family and social support system. Communication abilities may be diminished, and tragically, many residents face the distress of memory loss or cognitive decline. This convergence of losses can profoundly impact mental well-being and diminish residents’ zest for life.
RNPs provide a proactive strategy to assist residents in regaining or maintaining aspects of their independence. While the victories achieved through restorative programs—such as regaining the ability to walk unaided or manage personal dressing—might seem modest compared to the grief experienced, they hold immense value for a resident’s overall well-being. Beyond the personal benefits for residents, long term care facilities can also realize financial benefits through reimbursement and demonstrate documented evidence of delivering high-quality care.
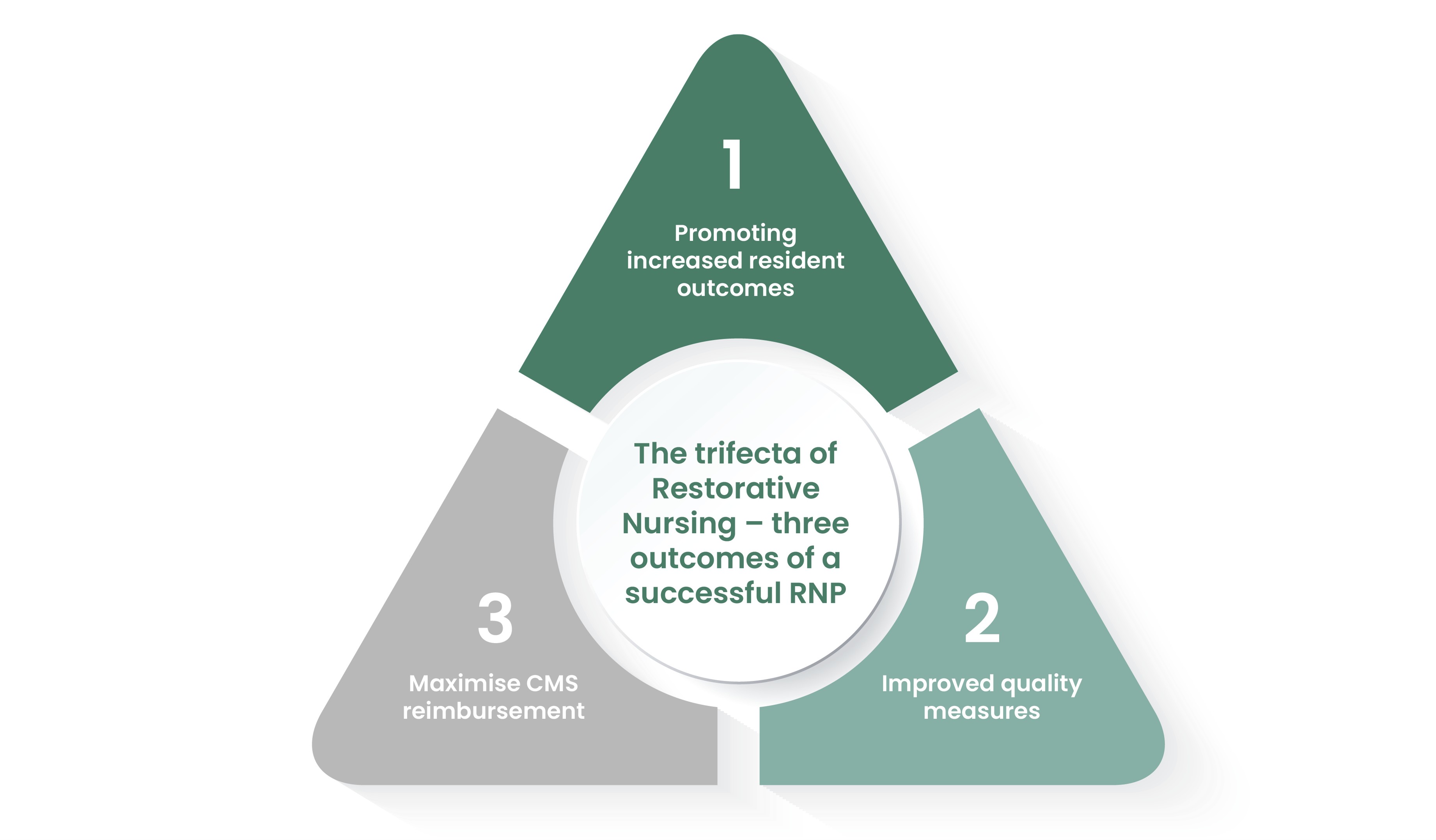 Trifecta of restorative nursing showcasing benefits for residents, staff, and facility in long term care
Trifecta of restorative nursing showcasing benefits for residents, staff, and facility in long term care
Types of Restorative Nursing Programs in Long Term Care
All restorative programs in long term care are designed to foster either the maintenance or improvement of residents’ functional abilities. However, they are broadly categorized into two primary types: Technique Programs and Training and Skill Practice Programs.
Technique Programs
Technique programs are specifically designed to maintain joint flexibility and range of motion in residents. Within this RNP category, nursing staff actively perform the activities either with or for the resident. Examples of technique-based programs commonly used in long term care include:
- Splint Assistance Programs: Aiding residents with splint application and ensuring proper usage to maintain joint function.
- Range of Motion (ROM) Improvement Programs: Systematic exercises conducted by staff to prevent stiffness and improve mobility in joints.
These programs are crucial for residents in long term care who may have limited mobility or are at risk of developing contractures, ensuring they maintain as much physical comfort and flexibility as possible.
Training and Skill Practice Programs
Training and skill practice programs in restorative nursing within long term care settings focus on enabling residents to perform activities themselves, with varying levels of support. In these programs, residents actively engage in tasks with verbal cues, direct supervision, or task segmentation provided by the staff. Examples of training and skill practice RNPs relevant to long term care include:
- Toileting Programs: Assisting residents to regain or maintain independence in toileting through scheduled routines and adaptive equipment.
- Communication Programs: Strategies to improve residents’ communication skills, including speech exercises or use of communication aids.
- Eating Programs: Techniques to help residents maintain or regain self-feeding skills, addressing issues like dysphagia or weakness.
- Walking Programs: Encouraging and assisting residents to walk safely, often utilizing mobility aids and structured walking schedules.
- Transfer Programs: Training residents in safe transfer techniques, such as moving from bed to chair, to enhance independence and reduce fall risks.
- Dressing and Grooming Programs: Teaching or re-teaching skills needed for personal care, promoting dignity and self-esteem.
A common example in many facilities is a “walk-to-dine” program, where residents are motivated and supported to walk from their rooms to the dining area for meals, promoting both physical activity and social engagement within the long term care environment.
Regulatory Impact of RNPs on Long Term Care Facilities
The success of Restorative Nursing Programs (RNPs) in enhancing residents’ quality of life in long term care settings has a direct, positive correlation with how regulatory bodies assess a facility’s quality measures.
According to Nicole Watson, “surveyors are going to do a record review of section GG to see their prior functioning which captures the resident’s usual ability to perform self-care, indoor mobility, how they manage stairs and their cognitive state prior to their illness, exacerbation or injury. Then they can compare our evaluation and the resident’s progress towards their goals.”
This scrutiny means that well-executed and consistently applied RNP programs not only improve resident outcomes but also significantly bolster a facility’s standing during regulatory reviews. Watson further emphasizes the financial implications, stating, “So, when your team are educated and consistent with RNP programs, not only do the residents benefit from better quality of life, but the programs impact the bottom line financially with reimbursement which we receive from CMS.” Thus, RNPs are instrumental in achieving dual benefits: superior resident care and enhanced financial stability for long term care facilities.
Financial Reimbursement and Restorative Nursing Programs in Long Term Care
To be eligible for reimbursement through restorative nursing programs in long term care, certain criteria must be met. A facility must implement a minimum of two or more RNPs for each qualifying resident, with each program active for at least six days per week. For a day to be counted as an RNP day for reimbursement purposes, a minimum of fifteen minutes of documented restorative care must be provided within a 24-hour period. These fifteen minutes do not need to be continuous, allowing for flexibility in scheduling and care delivery. Effective communication between day and night shifts is crucial to ensure these time requirements are consistently met. It is important to note that only the time staff spends directly interacting with the resident in restorative activities can be counted towards reimbursement, and RNPs should not duplicate or overlap with the goals of a resident’s formal therapy program (such as physical, occupational, or speech therapy).
Group RNPs are permissible and can be efficient, with a recommended minimum ratio of four residents to one staff member. However, it is essential that the staff leading the group session is thoroughly aware of each resident’s individual RNP goals to ensure the group activities effectively support these personalized objectives.
Documentation is paramount for successful reimbursement. It must clearly demonstrate resident progress toward established goals, and a Licensed Practical Nurse (LPN) or Registered Nurse (RN) must provide regular supervision, documentation of program re-evaluation, and adjustments at least quarterly. Common reasons for denial of reimbursement for restorative nursing in long term care include:
- Insufficient Documentation: Failure to consistently document at least 15 minutes of RNP activity per day, for a minimum of six days a week.
- Lack of Measurable Goals: Absence of clearly defined, measurable goals within the resident’s care plan.
- Inadequate Evaluation: Evaluations that are not sufficiently thorough to demonstrate ongoing progress and program effectiveness.
As with many aspects of long term care nursing, meticulous documentation is key. When facilities accurately document the execution of their RNPs and demonstrate continuous resident improvement through regular evaluations, they can achieve a higher Case Mix Index (CMI), which subsequently leads to increased financial reimbursement.
Responsibilities for Implementing Restorative Programs in Long Term Care
Successful implementation and execution of restorative nursing programs in long term care require a collaborative effort from various members of the healthcare team. Key personnel involved in the supervision and execution of RNPs include:
- Certified Nurse Aides (CNAs): CNAs often play a crucial role in the daily execution of RNPs, spending significant time with residents and assisting with activities.
- Licensed Practical Nurses (LPNs) and Registered Nurses (RNs): LPNs and RNs are essential for supervising RNPs, documenting progress, and ensuring programs are regularly reviewed and adjusted as needed. They also sign off on results and conduct periodic evaluations.
- Recreational Therapists: These professionals can contribute to the planning of RNP activities, particularly those that enhance psychosocial function and engagement.
- Restorative Aides: In facilities that employ restorative aides, these specialists are directly involved in implementing and managing restorative programs under the guidance of nursing staff.
In addition to these roles, collaboration with therapy departments—Physical Therapy, Occupational Therapy, and Speech Therapy—is vital for planning comprehensive programs, selecting appropriate activities, and determining necessary tools and equipment. Consulting with the social work department can also provide valuable insights into a resident’s psychosocial function and identify areas for potential improvement within the RNP framework.
While LPNs or RNs are responsible for supervision, review, and documentation, CNAs and restorative aides often handle the majority of direct resident interaction and activity implementation, accumulating the required minutes of RNP engagement. Furthermore, the involvement of Resident Assessment Coordinators (RNACs) is crucial to ensure accurate documentation and appropriate coding on the Minimum Data Set (MDS), which is essential for regulatory compliance and reimbursement.
Integrating Restorative Programs into Daily Care Despite Staffing Challenges in Long Term Care
Addressing the concern of incorporating restorative programs into daily care amidst ongoing staffing shortages in long term care, Nicole Watson, a respected expert in RNPs, offered an encouraging perspective during a recent webinar on restorative nursing. She stated, “Absolutely! That’s what I’ve always done because this staffing crisis didn’t just happen with Covid; it started prior.”
Watson provided a practical example related to dressing and grooming: “So, for dressing and grooming, for example, we need to set things up for Mary. We get all of her supplies ready and she’s getting herself dressed and she’s doing active range of motion. As long as the licensed nurse is outlining that dressing can be part of active range of motion, then we can incorporate that into the RNP and capture those minutes.”
This approach underscores the importance of recognizing and documenting restorative elements already present in routine care tasks. Watson emphasizes, “Sometimes we don’t take credit for the things that we’re doing and we just have to be smarter about how we’re doing it and have the documentation to support that.”
Creativity in designing RNP activities is key. Many long term care facilities are likely already performing activities that align with restorative program goals. The shift lies in intentionally structuring these activities, clearly defining goals, setting time expectations, and ensuring proper documentation to meet SMART (Specific, Measurable, Achievable, Relevant, Time-bound) criteria. By integrating restorative principles into existing workflows, long term care facilities can effectively enhance resident care and qualify for reimbursement, even under staffing constraints.
Final Thoughts on Restorative Programs in Long Term Care
While restorative nursing may sometimes be overshadowed by more immediate concerns in the demanding environment of long term care communities, it is crucial to recognize its profound value. Restorative Nursing Programs (RNPs) are not only vital for enhancing the current and future quality of life for residents but also for ensuring the financial health and sustainability of long term care facilities. Even in settings where restorative nursing is already prioritized, challenges in successful implementation and reimbursement can arise.
Resident engagement is pivotal to the success of an RNP. If a resident is unwilling to participate from the outset, the program’s effectiveness is likely to be limited. Furthermore, some residents may not be suitable candidates for restorative programs, complicating the mandate to have two programs in place for reimbursement eligibility. The complexities of program requirements and documentation can also pose logistical challenges for already stretched staff with varied schedules.
Despite these challenges, the commitment to providing the highest quality of care and improving the quality of life for our elders remains paramount. With this in mind, RNPs are indispensable for ensuring optimal care delivery and for the long-term viability of organizations dedicated to long term care.
For those seeking deeper insights, the full webinar presented by Nicole Watson offers extensive information and is accessible on the Accora website. Additionally, a comprehensive Q&A transcript from the webinar is available for further reading.
[