Introduction
The period immediately following a hospital stay is often fraught with challenges for patients. Alarmingly, about one in five individuals experience adverse events, such as medication complications or infections acquired in the hospital, during this vulnerable time. A significant consequence of these post-discharge issues is hospital readmission, with nearly 20% of older adults on Medicare being readmitted within 30 days of their initial discharge. This revolving door phenomenon not only impacts patient well-being but also places a substantial burden on the healthcare system.
Understanding What Is A Transition Care Program is crucial in addressing this issue. Essentially, transition care programs are designed to bridge the gap between hospital and home, or other healthcare settings. They represent a coordinated set of actions designed to ensure patients move safely and smoothly between different levels of care and healthcare providers. These programs aim to proactively manage potential risks during these transitions, particularly focusing on preventing adverse drug events (ADEs) and other complications that commonly lead to readmissions. ADEs are particularly concerning, with studies showing they contribute to nearly 100,000 hospitalizations among elderly patients annually.
Patients with neurological conditions, such as stroke, are particularly vulnerable during transitions of care. They face an elevated risk of recurrent events, disability, and even mortality. Therefore, for neurohospitalists, ensuring seamless and safe transitions for patients with conditions like stroke, epilepsy, and multiple sclerosis is a paramount patient safety concern.
Recognizing the financial and quality-of-care implications of readmissions and adverse events, national healthcare policies have increasingly emphasized the importance of improving transitional care. The Centers for Medicare & Medicaid Services (CMS) already monitors and publicly reports hospital readmission rates for conditions like pneumonia, heart attack, and heart failure, with potential penalties for hospitals with high readmission rates. It is anticipated that neurological conditions will soon be included in these measures. Initiatives like the Partnership for Patients have further underscored the need to enhance transitional care as a key strategy for reducing healthcare costs and improving patient outcomes.
While targeted transitional care approaches have shown some success for conditions like heart failure and COPD, effective strategies for neurological diseases remain less defined. Although research has explored various interventions, their impact on readmissions, emergency department visits, and post-discharge adverse events, especially in neurology, is still being investigated.
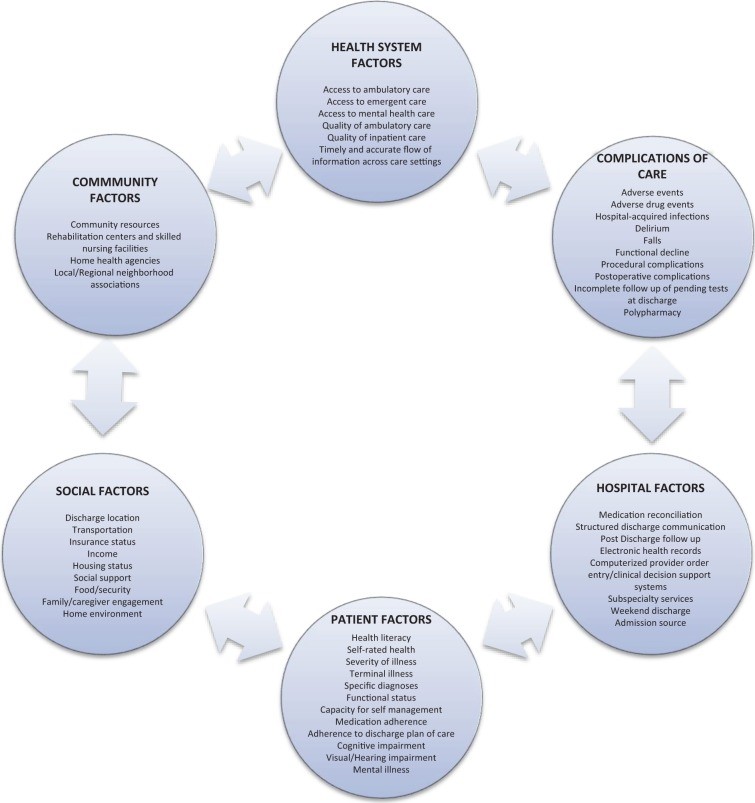
A significant portion of 30-day readmissions are considered preventable, often linked to factors outside the hospital setting, such as inadequate social support, financial constraints, and limited access to outpatient care (Figure 1). A review of stroke and cerebrovascular disease discharges highlighted that over half of readmissions were potentially avoidable, pointing to issues in care coordination, follow-up timing, and discharge instructions. Despite these challenges, overall readmission rates have shown a downward trend, indicating that progress in prevention is possible.
 Factors involved in hospital readmission
Factors involved in hospital readmission
Figure 1. Understanding the multifaceted factors contributing to hospital readmission is crucial for effective intervention strategies.
In today’s healthcare landscape, where value-based care is paramount, transitional care programs represent a high-value approach. While requiring resource investment, these programs align with the core values of neurohospitalists and the needs of patients by prioritizing patient safety and strengthening the connections within the healthcare system. This review delves into the nature of transitional care strategies, analyzes the effectiveness of existing programs, and provides specific recommendations for neurohospitalists to implement impactful transition care.
Defining Transition Care Strategies and Adverse Events
To fully grasp what is a transition care program, it’s essential to define its core components and the issues it aims to address. A “transitional care strategy” is best understood as a structured intervention, or a combination of interventions, initiated during a hospital stay, specifically designed to facilitate a safe and effective patient transition from one care setting to another – most commonly from hospital to home.
These strategies are often categorized into three main types based on timing of intervention:
- Predischarge interventions: These are actions taken while the patient is still in the hospital. Examples include assessing readmission risk, patient and caregiver education, creating personalized discharge plans, coordinating communication with outpatient providers, involving multidisciplinary discharge teams, assigning dedicated transition providers, and medication reconciliation.
- Postdischarge interventions: These occur after the patient has left the hospital. They can include proactive patient outreach through phone calls or home visits, facilitating timely clinical follow-up appointments, and post-discharge medication reconciliation.
- Bridging interventions: These are the most comprehensive, incorporating elements of both predischarge and postdischarge care. They provide continuous support and monitoring throughout the transition period.
Table 1 provides a detailed taxonomy of these interventions:
Table 1. Taxonomy of Interventions to Improve Transitional Care at Hospital Discharge.
| Predischarge interventions | Assessment of risk of adverse events or readmissions |
|---|