The healthcare landscape is constantly evolving, with hospitals facing increasing pressure to optimize patient care and reduce readmission rates. A critical area of focus in recent years has been transitional care. But what is a transition care program and why is it so important? This article delves into the concept of transition care programs, exploring their definition, the risks they address, effective strategies, and key recommendations for healthcare professionals aiming to improve patient outcomes and safety during the vulnerable period following hospital discharge.
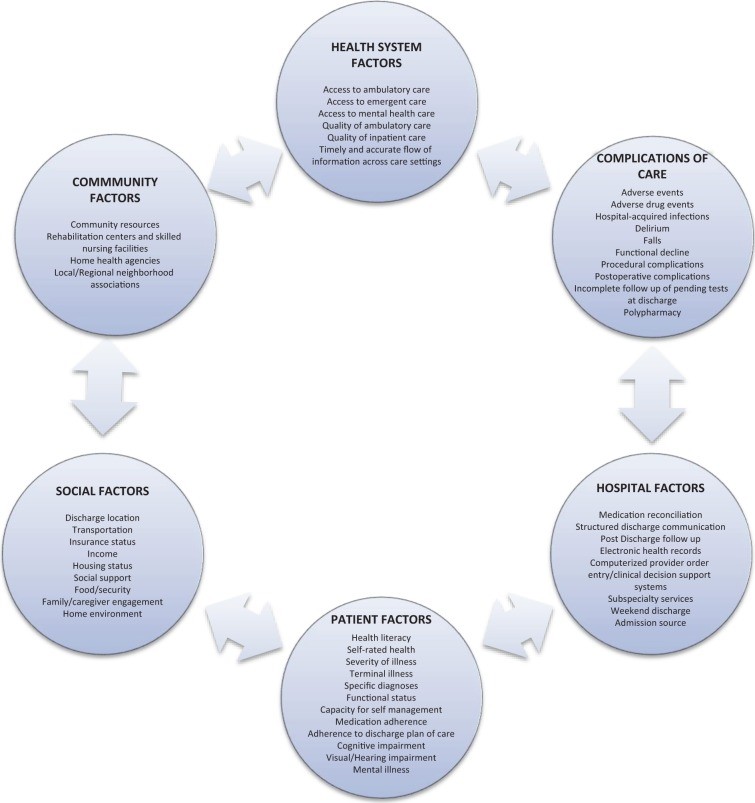
Figure 1: Key factors contributing to hospital readmission, including both in-hospital care elements and external factors like social support and access to care.
Understanding Transition Care: Bridging the Gap Between Hospital and Home
The period immediately following hospital discharge is often fraught with challenges for patients. Studies reveal that a significant proportion of patients experience adverse events, such as medication complications or hospital-related infections, within the weeks after leaving the hospital. Alarmingly, a substantial number of older patients are readmitted to the hospital within just 30 days of discharge. These statistics highlight a crucial gap in healthcare delivery – the transition from inpatient to outpatient care.
Transition care programs are specifically designed to address this gap. They represent a coordinated set of actions created to ensure patient safety and well-being as individuals move between different healthcare settings and providers. This transition, often from a hospital to home, or to other outpatient services, requires careful planning and execution to minimize risks and promote a smooth recovery. Effective transition care aims to “bridge” these care gaps, ensuring continuity and reducing the likelihood of adverse events and unnecessary hospital readmissions.
The need for robust transition care programs is further underscored by national policy initiatives. Organizations like the Centers for Medicare & Medicaid Services (CMS) are increasingly focusing on hospital readmission rates as a key indicator of healthcare quality. Hospitals with high readmission rates may face financial penalties, incentivizing the implementation of effective strategies to improve post-discharge care. This mandate for improvement emphasizes the critical role of transition care programs in the modern healthcare system.
While disease-specific transition care strategies have shown some success in conditions like heart failure and respiratory illnesses, understanding and implementing effective programs for neurological conditions, such as stroke, remains a critical area of focus. Neurological patients often face complex and chronic conditions, making them particularly vulnerable during care transitions.
Defining Transition Care Strategies and Post-Discharge Adverse Events
To effectively implement and evaluate transition care programs, it’s essential to clearly define the key components and outcomes. A transition care strategy is defined as a specific intervention or a combination of interventions initiated before a patient leaves the hospital. The primary goal is to facilitate a safe and effective transition from the hospital setting to the patient’s next destination, most commonly their home.
These strategies can be categorized into three main types:
- Predischarge Interventions: Actions taken while the patient is still in the hospital, aimed at preparing them for discharge and the subsequent care.
- Postdischarge Interventions: Support and follow-up provided to the patient after they have left the hospital, ensuring ongoing care and addressing any emerging issues.
- Bridging Interventions: Programs that incorporate elements of both predischarge and postdischarge care, creating a continuous bridge across the transition period. These are often considered the most effective approach.
Table 1. Taxonomy of Interventions to Improve Transitional Care at Hospital Discharge.
| Predischarge interventions | Assessment of risk of adverse events or readmissions |
|---|---|
| Patient engagement (eg, patient or caregiver education) | |
| Creation of an individualized patient record (customized document in lay language containing clinical and educational information for patients’ use after discharge) | |
| Facilitation of communication with outpatient providers | |
| Multidisciplinary discharge planning team | |
| Dedicated transition provider (who has in-person or phone contact with the patient before and after discharge) | |
| Medication reconciliation | |
| Postdischarge interventions | Outreach to patients (including follow-up phone calls, patient-activated hotlines, and home visits) |
| Facilitation of clinical follow-up (including facilitated ambulatory provider follow-up) | |
| Medication reconciliation after discharge | |
| Bridging interventions | Inclusion of at least 1 predischarge component and at least 1 postdischarge component |
Table 1: Breakdown of different intervention types used in transition care programs, categorized by timing and focus.
Post-discharge adverse events are defined as negative patient experiences that occur after hospital discharge and are clinically significant. These can include:
- New or worsening symptoms.
- Abnormal lab results requiring changes in treatment.
- Injuries such as adverse drug events (ADEs), falls, or hospital-acquired infections that are linked to hospital care.
Hospital readmission itself is also often considered a significant adverse event, commonly measured at 30-day, 60-day, 90-day, and 6-month intervals following the initial hospitalization.
Identifying Patients at Risk: Who Benefits Most from Transition Care Programs?
While predicting exactly which patients will experience readmission or adverse events is complex, certain populations are known to be at higher risk during the post-hospitalization period. These include:
- Older adults: Age is a significant risk factor due to increased frailty, polypharmacy, and prevalence of chronic conditions.
- Chronically ill patients: Individuals with multiple chronic conditions often require complex care and are more vulnerable to complications after discharge.
- Stroke patients: Patients recovering from stroke face a heightened risk of recurrent strokes, disability, and other complications.
Factors like poor functional status at discharge, psychiatric illness, and limited social support also contribute to increased risk. Although standardized risk prediction models are still evolving, healthcare providers can proactively identify high-risk individuals and prioritize them for enrollment in transition care programs.
Key Strategies in Effective Transition Care Programs: Learning from Successful Models
Several well-established transition care programs have demonstrated effectiveness in reducing readmissions and improving patient outcomes. These programs offer valuable insights into successful strategies and common elements. Four prominent models are:
Table 2. Highlighted Hospital-Based Transitional Care Programs.
| Programs | Strategies | Description/Effectiveness |
|---|---|---|
| Care Transitions Intervention40–43 | Patient engagement Individualized patient record Dedicated transition provider Facilitation of communication to outpatient providers Outreach Medication reconciliation | Focuses on 4 domains of care including self management skills. Studied in several settings. CCT40,43 and RCT41,42. Decreased 30-day readmission rates: ARR 4.9%,40 ARR 3.6%,41 and ARR 5.8%43. Decreased 90-day readmission rates: ARR 5.8%41 and ARR 21.7%42. 30-Day ED visits: ARR 3.2% (NS)40 |
| Transitional Care Model44–47 | Patient engagement Individualized patient record Dedicated transition provider Facilitation of communication to outpatient providers Facilitated clinical follow-up Outreach | Nurse-led program studied in geriatric patients, intensive outreach with home and telephone follow-up. RCT. Decreased 90-day readmission rates: ARR 16.8%44 (within 24 weeks), ARR 48.0%,45 and ARR 13%46 (within 6 weeks). ED visits (within 24 week): NS44,47. Adverse events (postdischarge infection) ARR 16.7% (NS)45 |
| Project RED48 | Patient engagement Individualized patient record Dedicated transition provider Facilitation of communication to outpatient provider Multidisciplinary team Outreach Medication reconciliation (predischarge and postdischarge) | Team-based program included pharmacist outreach and medication reconciliation. RCT. Decreased 30-day readmission rates: ARR 5.8% (NS). Decreased 30-day ED visits: ARR 8.0% |
| Project BOOST49 | Patient engagement Multidisciplinary team Outreach Medication reconciliation Risk assessment | Multicenter QI program with mentored implementation. CCT49 and pre–post study51. Decreased 30-day readmission rates: ARR 2%51 and ARR 5.9%49 |
Table 2: Overview of prominent hospital-based transition care programs, highlighting their strategies and effectiveness in reducing readmissions and ED visits.
Care Transitions Intervention (CTI)
Developed by Eric Coleman, the Care Transitions Intervention focuses on empowering patients to actively manage their health after discharge. Key components include:
- Medication Management: Ensuring patients understand their medications and how to take them correctly.
- Personal Health Record: Creating a portable record for patients to track their health information across different care settings.
- Follow-up Appointments: Facilitating timely follow-up with primary care providers.
- “Red Flag” Recognition: Educating patients to identify warning signs and know when to seek medical attention.
A “transition coach,” often an advanced practice nurse, provides home visits and phone support, emphasizing patient engagement and self-management skills. CTI has demonstrated significant reductions in 30-day readmission rates across various healthcare settings.
Transitional Care Model (TCM)
Pioneered by Mary Naylor, the Transitional Care Model is a nurse-led program specifically designed for high-risk, chronically ill older adults. A transitional care nurse (TCN) plays a central role, following patients from the hospital to home and providing:
- Discharge Planning: Coordinating care and resources before the patient leaves the hospital.
- Home Visits and Phone Follow-up: Providing ongoing support and monitoring in the post-discharge period.
- Communication Facilitation: Ensuring seamless communication between hospital and outpatient providers.
TCM emphasizes a multidisciplinary approach, with the TCN collaborating with physicians, social workers, and pharmacists. Studies have shown significant reductions in readmission rates at 60 and 90 days using the TCM.
Project Reengineered Discharge (RED)
Project RED focuses on a multidisciplinary, team-based approach to discharge planning, coordinated by a nurse discharge advocate (DA). Key elements include:
- Patient Engagement: Actively involving patients in the discharge planning process.
- Individualized Post-Hospitalization Plan: Providing patients with clear, illustrated instructions for their care at home.
- Pharmacist Follow-up: A pharmacist conducts telephone follow-up, including medication review and communication with the primary care provider.
Project RED has demonstrated significant reductions in hospital utilization, including both readmissions and emergency department visits.
Project Better Outcomes for Older Adults Through Safe Transitions (BOOST)
Project BOOST, supported by the Society of Hospital Medicine, is a quality improvement collaborative that helps hospitals implement effective transition care programs. It provides a toolkit and mentorship to guide hospitals in developing site-specific programs. Key components of BOOST include:
- Risk Assessment: Identifying patients at high risk for readmission.
- Medication Reconciliation: Ensuring accurate medication lists and addressing discrepancies.
- Discharge Checklist: Using a checklist to ensure all essential discharge tasks are completed.
- Multidisciplinary Team Approach: Involving various healthcare professionals in the discharge process.
Project BOOST has shown modest reductions in readmission rates across various hospitals.
Strategies Tailored for Neurologic Patients
While the programs above are broadly applicable, specific strategies can be tailored for patients with neurological conditions like stroke. Research suggests that interventions focused on care coordination in the hospital can improve outcomes for stroke patients. Specific interventions that have shown promise include:
- Secondary Stroke Prevention: Ensuring patients are on appropriate medications to prevent future strokes (antithrombotics, antihypertensives, lipid-lowering agents).
- Dysphagia Screening: Identifying and managing swallowing difficulties to prevent complications like pneumonia.
- Reducing Urinary Catheter Use: Minimizing catheter use to prevent catheter-associated urinary tract infections.
Neurohospitalists are uniquely positioned to implement these targeted interventions and improve the quality of care for their patients beyond the hospital stay.
Common Threads in Successful Transition Care Programs
Despite variations in their specific approaches, successful transition care programs share several common features:
- Bridging Interventions: Most effective programs incorporate both predischarge and postdischarge components, creating a continuous link between hospital and home.
- Dedicated Transition Provider: A designated individual, often a nurse or case manager, serves as a point of contact and care coordinator throughout the transition.
- Patient Engagement and Outreach: Programs prioritize actively involving patients and caregivers in their care and provide proactive outreach after discharge.
- Improved Communication: Focus on enhancing communication across different healthcare settings and providers.
These common elements highlight the importance of a coordinated, patient-centered approach to transition care.
Implementing Transition Care Programs: Considerations and Costs
While the benefits of transition care programs are evident, successful implementation requires careful consideration of resources, costs, and sustainability. Detailed information on the cost-effectiveness and resource utilization of different programs is still needed to guide hospitals in making informed decisions about implementation.
Discussion: The Value of Transition Care and Future Directions
Transition care programs represent a vital strategy for improving patient safety and reducing hospital readmissions. The evidence from established models like CTI, TCM, Project RED, and Project BOOST underscores the effectiveness of bridging interventions and dedicated transition providers. While these programs may require significant resources, the potential benefits in terms of reduced readmissions, improved patient outcomes, and avoidance of financial penalties make them a worthwhile investment for hospitals and healthcare systems.
Further research is needed to better understand the specific impact of these programs on patients with acute neurological illnesses and to optimize implementation strategies for diverse hospital settings. Focusing on cost-effectiveness, sustainability, and tailoring programs to specific patient populations will be crucial for maximizing the impact of transition care in the future.
Recommendations for Neurohospitalists: Leading the Way in Transition Care
Neurohospitalists are uniquely positioned to champion and implement effective transition care programs. To improve patient care transitions and reduce readmissions, neurohospitalists should consider the following recommendations:
Table 3. Summary Recommendations for the Neurohospitalist.
| Obtain data on 30-day readmission rates (all cause and disease- or unit-specific rates) |
|---|
| Consider your hospital’s quality improvement and patient safety infrastructure—electronic health record, prior experience with quality improvement initiatives |
| Create a interdisciplinary team and find champions |
| Identify outcomes to measure (30-day readmission rates, adverse drug events, or medication errors) |
| Implement a bundled (multicomponent) strategy that includes patient engagement, transitions provider, medication reconciliation, facilitation of communication, and patient outreach |
| Incorporate disease-specific interventions (secondary stroke prevention and dysphagia screening) |
Table 3: Key recommendations for neurohospitalists to effectively implement and lead transition care initiatives within their hospitals.
- Data-Driven Approach: Begin by analyzing hospital-specific readmission rates to understand the scope of the problem and identify areas for improvement.
- Leverage Existing Infrastructure: Assess the hospital’s current quality improvement resources and electronic health record capabilities to support program implementation.
- Build an Interdisciplinary Team: Create a team of champions from various disciplines to drive the development and implementation of transition care programs.
- Measure Key Outcomes: Track relevant metrics such as readmission rates, adverse drug events, and medication errors to evaluate program effectiveness.
- Implement Multicomponent Strategies: Adopt bundled approaches incorporating patient engagement, transition providers, medication reconciliation, communication facilitation, and patient outreach, drawing inspiration from successful models.
- Incorporate Disease-Specific Interventions: For neurological patients, integrate targeted interventions such as stroke prevention measures and dysphagia screening.
By taking a proactive and evidence-based approach, neurohospitalists can play a pivotal role in enhancing transition care, improving patient safety, and optimizing healthcare outcomes in the crucial post-hospitalization period.
Footnotes:
Authors’ Note: All statements expressed in this work are those of the authors and should not in any way be construed as official opinions or positions of the University of California, San Francisco, AHRQ, or the US Department of Health and Human Services.
Declaration of Conflicting Interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article. Stephanie Rennke is a consultant for the Society of Hospital Medicine’s Project BOOST.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported in part by funding from the Agency for Healthcare Research and Quality (AHRQ), US Department of Health and Human Services (contract no. HHSA-290-2007-10062I).
References