Neurological diseases represent a significant and growing public health challenge. The stark reality is that nervous system disorders, including conditions like Alzheimer’s disease, Parkinson’s disease, autism spectrum disorders, and amyotrophic lateral sclerosis (ALS), will impact nearly everyone, either directly or indirectly, during their lifetime. This widespread impact underscores the critical importance of understanding What Public Health Care Programs Concerning The Nervous System are available, how they can be improved, and what research is paving the way for more effective interventions.
Scientists at leading institutions like the Harvard Stem Cell Institute (HSCI) are deeply engaged in unraveling the complexities of neurological diseases. Their research highlights the interconnectedness of the nervous system with other bodily systems, revealing that conditions originating outside the brain, such as those related to blood, metabolism, and even gut health, can profoundly affect neurological health. Conversely, nervous system disorders can impact these peripheral systems. This intricate relationship emphasizes the need for comprehensive public health approaches that consider the whole body when addressing nervous system health.
A Multifaceted Approach to Nervous System Diseases
Alzheimer’s disease serves as a prime example of the challenges in treating neurological conditions and the necessity for robust public health care programs. Despite numerous therapeutic attempts, effective treatments remain elusive, partly because Alzheimer’s is influenced by a multitude of factors. This complexity underscores the need for public health strategies that go beyond simple treatment models and embrace prevention, early detection, and comprehensive care management.
However, there is significant hope. Research indicates that neural tissues possess a remarkable capacity for repair, even when damaged by disease, injury, or aging. Public health initiatives can leverage this knowledge by focusing on strategies that promote neural repair and cognitive function improvement, rather than accepting cognitive decline as irreversible. This optimistic perspective is crucial for shaping effective public health care programs aimed at mitigating the impact of nervous system diseases.
The principles guiding Alzheimer’s research at HSCI are applicable across the spectrum of neurological diseases. By adopting innovative approaches and fostering a deeper understanding of these conditions, researchers aim to accelerate the development of better treatments and, importantly, inform the creation of more effective public health care programs for nervous system disorders.
The Critical Role of Systemic Health in Neurological Well-being
The health of the nervous system is inextricably linked to overall bodily health. Lifestyle factors such as exercise, diet, and stress management are known to influence cognitive aging. Even seemingly minor systemic insults, like a common cold or the effects of anesthesia, can exacerbate cognitive decline in individuals with neurological diseases. This highlights the public health relevance of promoting healthy lifestyles as a preventative measure against neurological decline.
Groundbreaking research in older mice has shown that exposure to younger blood can rejuvenate aged tissues. This suggests the presence of circulating factors in blood capable of repairing damage caused by disease, injury, or aging. Identifying and harnessing these factors could revolutionize public health approaches to neurological diseases, potentially leading to preventative therapies or early interventions delivered through public health programs.
These circulating factors, originating from outside the nervous system, can profoundly regulate central nervous system (CNS) function. Furthermore, they impact the brain’s vasculature, the critical interface between the brain and blood-borne elements. The strong bidirectional link between cardiovascular and metabolic diseases and neurological disorders emphasizes the need for integrated public health strategies that address these interconnected health challenges holistically. Public health care programs for nervous system diseases must consider and address these broader systemic connections.
Recognizing these intricate connections, HSCI’s research program fosters collaboration among experts across various bodily systems, not just within neurology. This interdisciplinary approach is essential for deciphering the complex interplay between peripheral tissues and the brain, paving the way for more effective and comprehensive public health interventions.
Gut Health as an Early Indicator and Target for Public Health Programs
Emerging evidence points to the gut as a critical area of focus for understanding and potentially preventing nervous system diseases. Pathologies in the intestine have been observed decades before the onset of Parkinson’s disease. Chronic constipation, a common gastrointestinal issue, is recognized as an early warning sign for several nervous system disorders, often preceding the appearance of CNS symptoms. This temporal relationship raises a crucial question for public health: can addressing these early gastrointestinal symptoms prevent or delay the progression of brain-related symptoms?
Research is underway to determine the origins and progression of these diseases, investigating whether genetic mutations can simultaneously impact both the intestine and the brain. Analyzing electronic health records to identify correlations between Parkinson’s disease and earlier health issues could enable the development of predictive models and targeted public health screening programs for early risk detection and intervention. Public health initiatives focused on gut health and early detection could significantly alter the trajectory of nervous system diseases.
Human-Based Research: Transforming Public Health Strategies
While animal models, particularly mice, have provided valuable insights into neurological diseases, significant differences exist between human and mouse brains. The advent of human cellular models represents a transformative shift in neurological disease research and its implications for public health care programs.
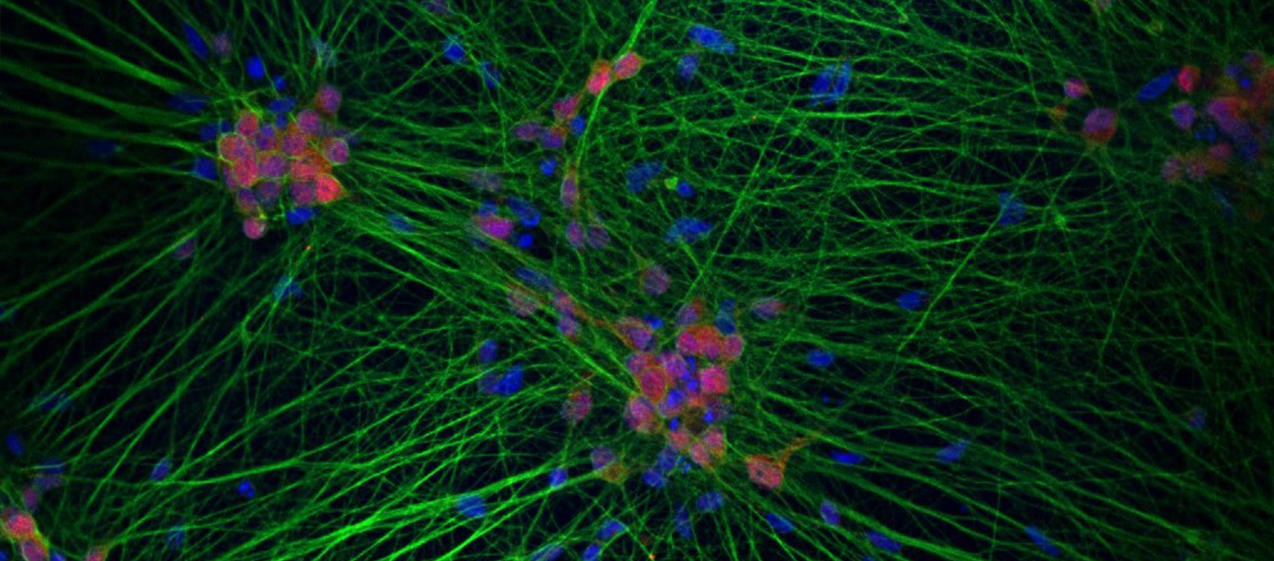
The ability to study neurological diseases using human neural tissue grown in the lab from patient-derived cells (iPSC-derived neurons) offers unprecedented opportunities. This human-centric approach allows researchers to investigate the effects of potential treatments and public health interventions directly on human cells, prior to clinical trials. This capability is invaluable for developing and refining public health strategies for diseases like Parkinson’s, ALS, Alzheimer’s, and other neurological conditions, ensuring that interventions are tailored to human biology.
Collaborative Science for Enhanced Public Health Impact
Addressing the complex challenges of nervous system diseases requires a collaborative, multidisciplinary approach, mirroring the interconnectedness of the body itself. The HSCI Nervous System Diseases Program exemplifies this by bringing together Harvard scientists with diverse expertise spanning:
- Blood vessel development
- Metabolic disease
- Neurological disease
- Bioengineering
This collaborative environment fosters the exchange of ideas, knowledge, data, and technology, accelerating progress towards effective public health solutions. By empowering scientists with cutting-edge tools, including iPSC technology, organoids, bioimaging, and electrophysiology, HSCI is pushing the boundaries of research and contributing to the development of innovative public health care programs. Furthermore, supporting the development of new research tools ensures continued advancement in this critical field.
Supporting Research to Strengthen Public Health Care Programs
Supporting research initiatives like the HSCI Neurological Diseases Program is a direct investment in strengthening future public health care programs for nervous system disorders. By advancing our understanding of these complex conditions, research paves the way for more effective prevention strategies, early detection methods, and targeted treatments that can be implemented through public health programs.
Contributions to this research not only accelerate scientific discovery but also expand the network of expertise and knowledge available to address nervous system diseases. This collaborative growth, leveraging the exceptional talent at Harvard and its affiliated hospitals, is essential for developing comprehensive and impactful public health care programs that can truly restore function and improve the lives of individuals affected by neurological diseases.